![]()
This month, I’ve decided to do a deep-dive into wearable skin temperature trackers. It’s my hope that this Info Hub will be a helpful, comprehensive resource for you to browse through should you be interested in purchasing a wearable skin temperature tracker for Fertility Awareness Based Method (FABM) charting.
Without fail, one of the most common questions I get in my direct messages on social media is “what do you think about so-and-so wearable tracking/fertility device or app?”.
This is no surprise given the growing popularity of fertility tracking devices, and the saturation of the femtech* market, with more new products and innovations being released each year.
Disclaimers:
- Details are correct to the best of my knowledge as at the time of writing this article in October 2022; however, the femtech industry moves quickly with constant innovation and device/app upgrades. Keep this in mind and always do your own due diligence if you’re interested in purchasing any sort of femtech device.
- I am not a “tech writer”. I use very minimal technology in my own FABM charting practise. Not only that but I also prefer to paper chart, and I manufacture and sell beautiful charting journals which you can browse here. I’ve aggregated and summarised as much relevant info as I could find in this information hub, but I am not an authority or expert on emerging FABM charting technologies.
- I am not trained in statistical analysis or study analysis, so where I link to/discuss studies you are reading my personal opinion. If you’re a FABM enthusiast statistician I’m sure you can glean some interesting insights from some of the studies mentioned!
In addition, this information hub barely scratches the surface when it comes to wearable temperature trackers and is simply designed as a springboard for you to do your own further investigation on any topics that interest you. If you see something that is incorrect or should be changed, please let me know in the comments below.
Alright, let’s dive in!
*The term “femtech” is short for “female technology”. It refers to tools, technologies, services and software that aim to address women’s/menstruators’ health issues.
Click on each of the headings below to learn more. Start at the top and work your way down.
![]()
Basal body temperature (BBT) thermometers are designed to pick up very small fluctuations in body temperatures. BBT thermometers are more accurate than standard fever thermometers.
Most Symptothermal Methods require that you use a basal body temperature thermometer that displays two decimal places.
Here are some important parameters to keep in mind when you are searching for a thermometer to use with Symptothermal Methods:
Measuring accuracy and tolerance:
Measuring accuracy refers to how close your thermometer will measure to a known temperature. Measuring accuracy is usually stated as a tolerance which explains how far either side of a known temperature your thermometer might measure. BBT thermometers usually have an accuracy of +/-0.05°C / 0.1°F.
This means that if the known temperature is 36.53°C, your BBT thermometer may give you a reading anywhere between 36.48°C and 36.58°C.
Display resolution:
Display resolution refers to how many decimal places your thermometer/device displays. Basal body temperature thermometers should have a display resolution of one hundredth of a degree (0.01°C / 0.01°F).
Precision:
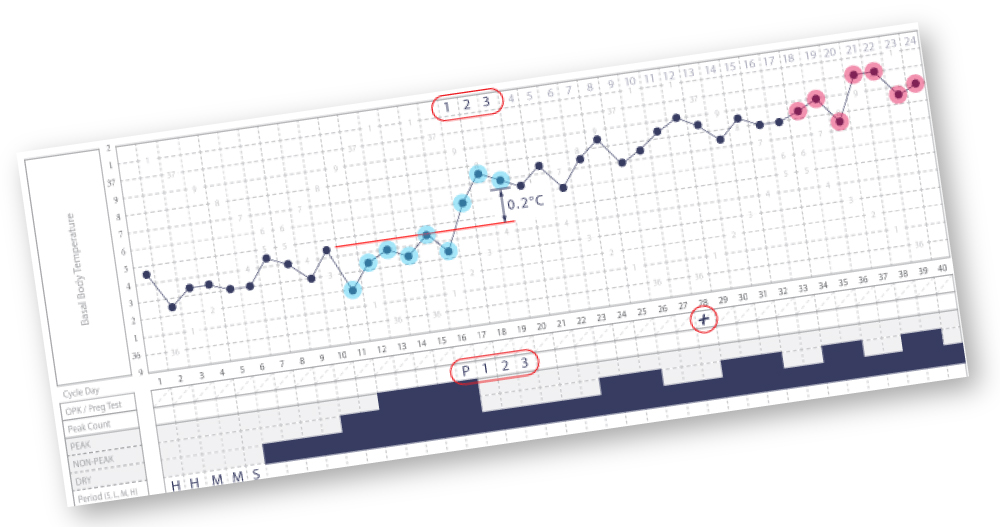
Precision refers to how consistent the results are when the measurement is repeated. When it comes to charting with the Symptothermal Method, precision is more important than accuracy. A highly precise thermometer might be slightly inaccurate, but the error in accuracy will be repeated every day of the menstrual cycle, meaning that we can confidently identify our temperature shift (knowing that a shift is not caused by an imprecise thermometer reading, but by our true rise in temperature after ovulation).
In other words, even if your BBT thermometer is slightly inaccurate this will not affect your charts so long as your thermometer is precise, and the error is consistent across the entire chart.
Core body temperatures refer to internal temperatures from our core (usually obtained via oral, vaginal or rectal sites for FABM charters).
Distal skin temperatures usually refer to skin temperatures taken from the hands and feet (wrists are included).
Proximal skin temperatures usually refer to skin temperatures taken from closer proximity to our core (such as our upper arms/thighs and stomach).
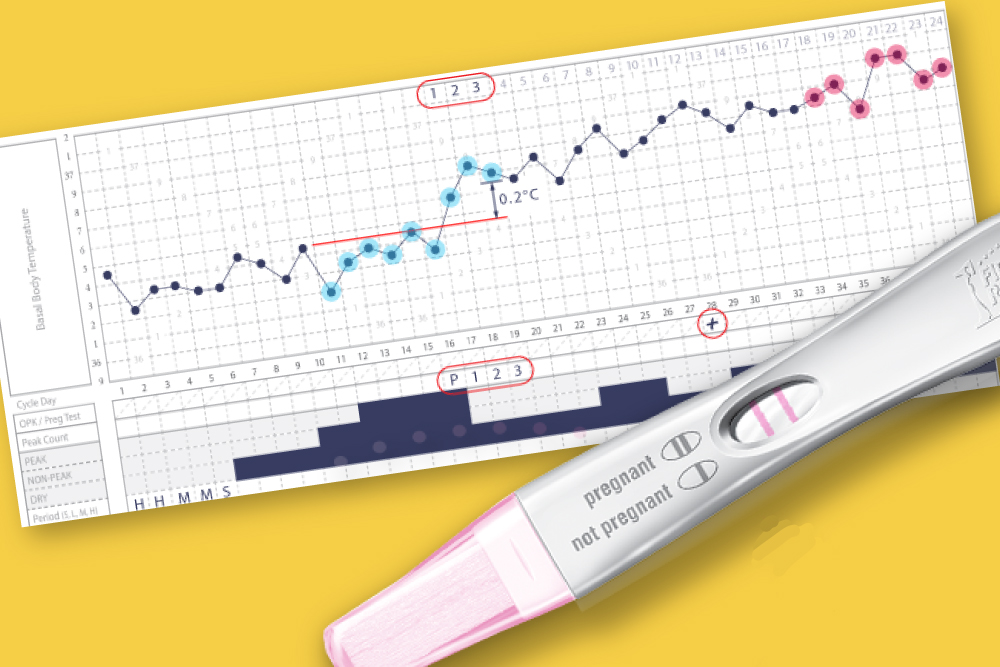
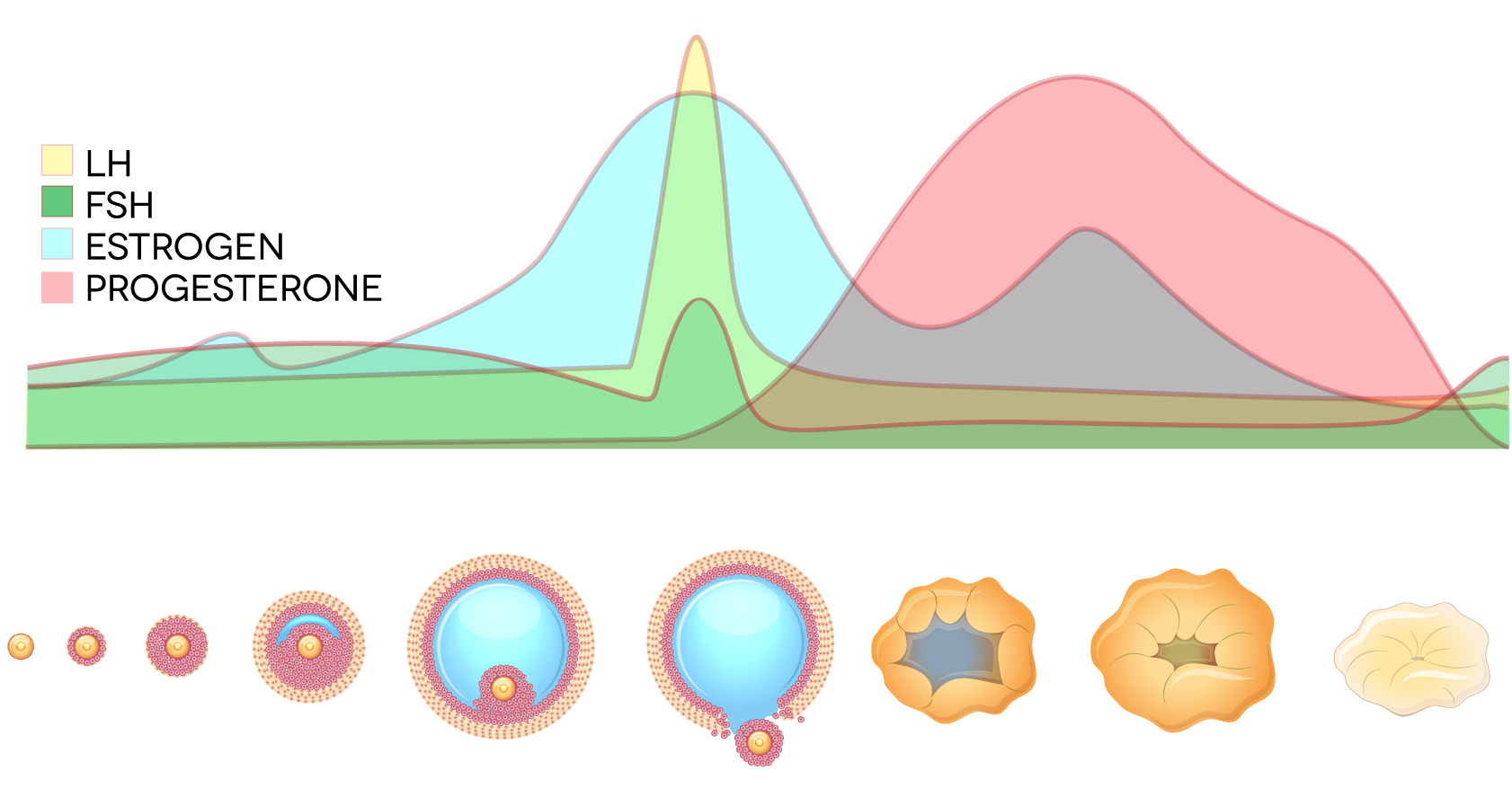
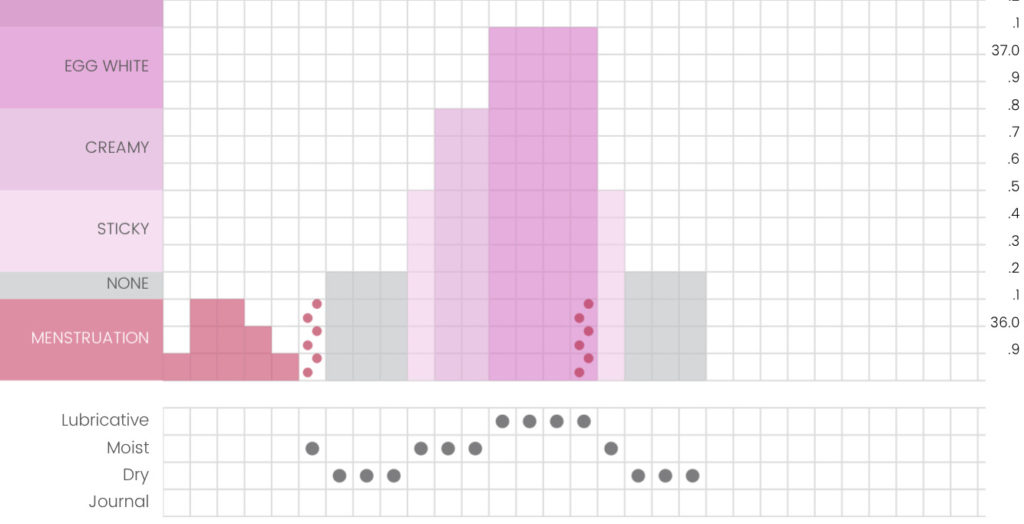
Basal body temperature (BBT) is our core body temperature at its lowest state while we are in a state of rest. This usually occurs at around 4am each morning. Basal body temperatures are important for Symptothermal Method charters because they usually rise for two weeks after ovulation has occurred, until our next period begins. This rise in temperature is due to a hormone called progesterone, which we release in large quantities in the two weeks after ovulation. Charting our temperatures (in conjunction with our cervical mucus) helps us to confirm that ovulation has passed. To learn how to do this, visit the Instructor Directory or visit the Self-Teaching page on this website.
Waking temperatures (either oral, vaginal or rectal) are used as a close approximation of true basal body temperature for Symptothermal Method charters. Taking our temperature as soon as we wake up saves us having to wake up at 4am each day.
The melatonin we produce sends signals to our distal skin regions (hands and feet) that create a rise in blood flow. This rise in blood flow is due to vasodilation (expansion of the veins that hold our blood).
With more blood flowing through these veins, we lose heat through the skin of our extremities.
The heat loss in our extremities gradually lowers our core body temperature during the night. Our core body temperature is usually lowest at around 4am in the morning.
During waking hours, our distal temperatures (hands and feet) are lower than our proximal temperatures (upper arms/thighs and stomach etc).
After we fall asleep, our distal temperatures rise significantly (via the process of vasodilation mentioned above). This rise causes distal temperatures to then match proximal temperatures closely throughout the night. After waking, distal temperatures then drop lower once again.
What does this mean for FABM charting? During the night while asleep, distal temperatures closely match proximal temperatures. Many FABM charters already successfully use proximal upper-arm temperatures via the Tempdrop device to accurately visualise and assess their temperature shifts. With the right technology, FABM charters will likely soon be able to successfully utilise distal skin temperatures for FABM charting, too.
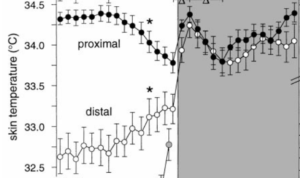
Distal and proximal skin temperatures do not follow this same circadian rhythm. Instead, they share an inverse relationship during wake times, before slowly converging to rise rapidly as sleep commences, before dipping around 2am and slowly rising back up again by around 5-6am.
Skin temperatures do not mirror core body temperatures during a single 24 hour circadian rhythm cycle. Despite this, they are still influenced by our changing hormones across our infradian menstrual cycle. They show a shift from lower temperatures prior to ovulation, to higher temperatures after ovulation. This means they can still be used to identify temperature shifts with FABMs (although to what level of contraceptive effectiveness, we don’t yet have a lot of evidence).
Some studies that have explored the biphasic properties of skin temperature across the menstrual cycle include:
- Chen W, Kitazawa M, Togawa T. Estimation of the biphasic property in a female's menstrual cycle from cutaneous temperature measured during sleep. Ann Biomed Eng. 2009;37(9):1827.
- Kräuchi K, Konieczka K, Roescheisen-Weich C, Gompper B, Hauenstein D, Schoetzau A, et al. Diurnal and menstrual cycles in body temperature are regulated differently: a 28-day ambulatory study in healthy women with thermal discomfort of cold extremities and controls. Chronobiol Int. 2014;31(1):102–13.
- Maijala, A., Kinnunen, H., Koskimäki, H. et al. Nocturnal finger skin temperature in menstrual cycle tracking: ambulatory pilot study using a wearable Oura ring. BMC Women's Health 19, 150 (2019).
- Alzueta E, de Zambotti M, Javitz H, Dulai T, Albinni B, Simon KC, Sattari N, Zhang J, Shuster A, Mednick SC, Baker FC. Tracking Sleep, Temperature, Heart Rate, and Daily Symptoms Across the Menstrual Cycle with the Oura Ring in Healthy Women. Int J Womens Health. 2022 Apr 8;14:491-503.
*Unfortunately, we do not have high quality clinical trial evidence of the accuracy of Tempdrop temperatures in the context of Symptothermal Method charting effectiveness. At present, we are relying more on the “social proof” of the many thousands of people currently using the Tempdrop to successfully identify biphasic temperature shifts during the menstrual cycle. The biphasic shift to a higher temperature is caused by the event of ovulation that occurs roughly 12-14 days prior to the onset of menstruation. Hopefully in future we will have more evidence not just on the Tempdrop but on all other skin-sensor wearables.
What does this mean? Most skin temperature-collection devices will need to filter temperatures through an algorithm that also tracks data collected about:
• Environmental temperatures
• Your body position
• Your activity level
• Your sleep status
As an example, the Tempdrop thermometer provides data based on proximal skin temperatures and is worn under the armpit close to the axillary artery. It measures skin temperatures with one sensor, ambient environmental temperatures with another sensor, and utilises a 3-axis accelerometer to track your body position, activity and sleep status. Data is then filtered through an algorithm to provide the most accurate skin temperature reading from the night. Most other skin-wearable thermometers have a similar approach.
Now that you’ve read through all of the above topics, you will have a better understanding of the relationship between our core body temperature, skin temperatures (both proximal and distal), and how these can be used for FABM charting.
If you’re curious to know more about some of the available products when it comes to wearable skin-temperature tracking devices, read on! For each device mentioned below, I have outlined key features plus my own personal opinion on its suitability for use with Symptothermal Method charting.
![]()
 Device: Tempdrop
Device: TempdropPrice: From USD $200
Type of skin temperatures (proximal or distal): Proximal
Skin site: Worn in an armband to collect underarm temperatures from near to the axillary artery.
Time worn: Worn only while sleeping
EMF exposure: The Tempdrop only emits EMFs while syncing with the Tempdrop app in the morning. EMFs are not released while being worn.
Associated app: Tempdrop syncs directly with the Tempdrop app. To view your temperatures, you must sync your Tempdrop with the Tempdrop app.
3rd Party integrations: Once you sync your Tempdrop with the Tempdrop app to retrieve your temperature, you can also auto-retrieve it into these additional apps on your phone: Chart Neo app, Read Your Body app, and OvuView app
Subscriptions required: None. You can choose to pay an annual subscription to the premium version of the Tempdrop app to access sleep data and automatic chart markings*.
Type of temperature data: Absolute values
Number of decimals: Two decimal places (.00)
Data points provided:
- Temperature
- Sleep data
The Tempdrop has the most “social proof” of any wearable skin temperature tracking device. They have over 10,000 users in their Facebook group and have been in use by FABM charters since 2017 now. I personally have successfully used the Tempdrop throughout my postpartum charting journey and am very happy with it.
I like the fact that the Tempdrop is only worn at night as I don’t like wearing things during the daytime (the only jewellery that I can wear 24-7 is a necklace, and even then I prefer taking it off while I shower). I like the fact that the Tempdrop is worn on the upper arm, as I don’t like wearing watches or rings while I sleep, because I sleep with my hands up near my face. This is just a personal idiosyncrasy though, and I’m sure most other people have no problem with watches and rings while sleeping!
I do sometimes wonder if the Tempdrop may be slightly *too* sensitive. In my personal experience, I believe it sometimes picks up the miniscule temperature rise that occurs during ovulation (there is a small amount of progesterone that is released during ovulation). With Sensiplan/NFPTA temperature rules (which make it relatively easy and straightforward to mark temperature shifts), I think this can sometimes result in a temperature shift being marked a day or two earlier than it would with oral temping. It’s possible that TCOYF charters (with their raised coverline), might not share this issue. Again, this is just my hypothesis based on a couple of my own personal charts. For Symptothermal Method users, cervical mucus observations should always be acting as a safety double-check regardless.
The Tempdrop device itself could probably benefit from some additional research and development to make it more user-friendly (especially when it comes to battery changes). I am glad that the algorithm no longer updates the most recent three temperatures, as this previously used to extend the time it takes to confirm a temperature shift in the luteal phase.You can read more of my thoughts about the Tempdrop here. I’m also an affiliate for the Tempdrop device and you can use my code TDLOVE29 to save 12% if you would like to purchase one.
At this point, I believe the Tempdrop remains the best choice for Symptothermal Method charters who cannot obtain oral/vaginal/rectal temperatures for some reason. That said, technologies are changing quickly - all it would take is for one of the other wearables listed here to begin showing accurate, absolute temperature values each morning and Tempdrop would have some serious competition (and I think that once BBRing is released, that will be the case!).
*I do not recommend anyone rely on automatic chart markings to evaluate their charts, especially if you are genuinely wanting to prevent unintended pregnancy. It's generally preferable to learn a method and understand how to mark your own charts.
 Device: Oura Gen3
Device: Oura Gen3Price: From USD $350
Type of skin temperatures (proximal or distal): Distal
Skin site: Worn in a ring to collect temperatures from the index, middle or ring finger.
Time worn: Recommended to be worn continuously. The Oura Gen3 ring is only taken off to charge, and battery can last up to 7 days. Despite this, Oura states that you can choose to wear it only at night if you prefer.
EMF exposure: The Oura Gen3 ring continuously emits low levels of electric and magnetic fields. The Oura Gen3 ring’s SAR level is 0.0003 W/kg. You can enable airplane mode inside the Oura app whenever you don’t need to look at your data (i.e. while you are sleeping).
Associated app: Oura app
3rd Party integrations: Apple Health, Google Fit, Strava, Natural Cycles (keep reading for my thoughts on Natural Cycles).
Subscriptions required: If you purchase a Gen3 Oura Ring, Oura Membership costs between 5.99 and 6.99 USD per month, depending on where you live in the world. Without a membership, you can still export your Oura data into CSV or JSON format from their web portal.
Type of temperature data: Temperatures are shown as fluctuations (+/-) from your personal “baseline temperature”. This is less useful for FABM charting, as we need an actual temperature value to plot on the graph section of our chart each morning.
Number of decimals: One decimal place (.0)
Data points provided:
- Temperature
- Sleep data
- Respiration/blood oxygen levels
- Resting heart rate
- Heart rate variability
I don’t really enjoy wearing jewellery on my hands (I almost never wear rings), so my immediate take is that it’s unlikely I would want to be wearing a ring 24-7. I also prefer products that I can buy outright, as opposed to subscription-based (especially with the cost of living rising a lot lately).
The only way currently to see an absolute temperature value each day is by using the Natural Cycles’ app. Read more here on why I don’t recommend Natural Cycles app for those who have a serious need to prevent pregnancy.
Interestingly, in Natural Cycles’ 510(k) premarket submission to the FDA to demonstrate that Oura temperatures are just as safe and effective as oral temperatures with the Natural Cycles app, they state: “Compared to the two-decimal place oral thermometer, the Natural Cycles algorithm provides additional 1.6 green days (not fertile) in the luteal phase of the menstrual cycle when the input temperature was from the Oura ring, without increasing the risk of unintended pregnancy”. I am interested to read more about this, but I cannot find the clinical study of the Oura Ring + Natural Cycles app. My initial reaction is that I am sceptical about this statement. Natural Cycles is already known for “confirming” temperature shifts a day or so earlier than Symptothermal Methods typically do (on the second day of a raised temperature for instance). For Oura Ring temperatures to then subtract an additional 1.6 days off the time it is taking Natural Cycles to confirm a temperature shift, gives me some pause for thought. Again, if you find this study please let me know – I searched high and low on the internet but could find no trace of it apart from its mention in Natural Cycles’ 510(k) FDA submission.
One thing that I do consider a drawcard is the absolute wealth of additional biometric information that Oura ring tracks and provides. If you’re going to spend a lot of money on a wearable device, this is definitely a beautiful premium option.
Overall, I think the Oura ring may have fantastic potential for future charters, provided they are able to begin delivering absolute temperature values (as opposed to fluctuation trends). This would mean FABM charters could use Oura temperatures in their chosen charting app or on their paper charts.
Studies (not an exhaustive list):
It is great to see a company such as Oura dedicating resources toward studying the accuracy of their device for menstrual cycle tracking. Despite this, I have found it difficult to access studies on exactly how accurate Oura temperatures are in comparison to oral waking temperatures for FABM charting. Data/studies that would be most relevant seem to be behind paywalls (Maijala et al., 2018) or I simply could not find them on the internet (Natural Cycles’ clinical study referenced in their 510(k) submission for FDA approval).
In saying this, Oura is the only company that is forthcoming with accuracy/precision figures on their website (this data is not available publicly for any other wearable skin temperature tracker that I researched). According to the Oura website, Oura is proven under laboratory conditions to be accurate to within 0.36°C (0.648°F). Remember that precision is arguably more important for FABM charting. Oura is proven under laboratory conditions to be precise to 0.13°C (0.234°F). It’s important to note that these are laboratory results and may not extend to real-world conditions.
It seems that if we really want reassurance of the comparability between Oura versus oral temperatures for FABM charting, we will need to engage in citizen science and make these comparison charts ourselves. This has definitely already begun in the FABM community, and as an example you can check out a comparison chart by Sensiplan teacher trainee Emma Lukkarila on her Instagram here.
You can also check out a great comparison between oral and Oura temperatures by fellow FABM Instructor Leslie Rewis in the FAM Support Facebook group here. Leslie's comparison is a great example of how distal temperature shifts seem to be more pronounced than oral/vaginal/rectal temperature shifts.
Maijala A, Kinnunen H, Koskimäki H, Jämsä T and Kangas M. Comparison of menstrual phases with nocturnal temperature of the Oura ring and oral body temperature at wake-up. World Congress on Medical Physics and Biomedical Engineering; 2018; Prague, Czech Republic: IUPESM; 2018:312–313.
- As far as I can see, this data actually compares Oura temperatures against oral temperatures, but is only available if you purchase the linked book for between AU $280 - $500. If anyone else has access to these findings I would be curious to read them: https://www.amazon.com/Congress-Medical-Physics-Biomedical-Engineering/dp/9811090378
- This study found that the accuracy of the Oura algorithm increased when the two study subjects with a BMI of over 30 were excluded from the calculations. Study authors state that a BMI of over 30 “is a potential confounder affecting distal skin temperature.” Other studies have shown that obesity causes distal temperatures to rise, to account for the insulating effect of a greater layer of subcutaneous abdominal fat. These higher distal temperatures allowed study participants to release heat and therefore regulate their core body temperature. Is it possible that a higher baseline distal temperature might mute the post-ovulatory rise in distal temperatures? I would love to see more studies on this in future (for both distal and proximal temperatures), as I have also heard some Tempdrop users speculate that their higher BMI may be impacting the accuracy of their temperature readings.
- Interestingly, the study authors also mention that smoking can impact skin temperature values. As the study was rather small (only 22 participants total) and none of them were smokers, it’s unclear whether this would be relevant for FABM charters.
- A third point which I found interesting is that distal skin temperatures showed a greater rise than oral temperatures in the luteal phase. Study authors state that the “Temperature difference [between follicular and luteal phases] was higher with skin temperatures than with oral temperatures.” On average, skin temperatures were 0.07 °C higher in the luteal phase. This gives me pause for thought as all Symptothermal temperature shift evaluation rules are based on oral/vaginal/rectal temperatures. It’s possible that the slightly higher rise in finger skin temperatures in the luteal phase might result in some temperature shifts being marked as “confirmed” earlier than they would with an actual FABM method. This is purely my own conjecture, but I think it would be an interesting topic for further study.
- This is probably one of the most interesting studies based on Oura temperatures that I have seen so far. Researchers found that changes over 2-5 hours in distal temperatures and heart rate variability predicted the onset of the luteinising hormone surge two days in advance for 100% of study participants. Fascinating! I imagine this could have notable benefit for real-time fertile window information for people who are trying to conceive, but would not provide enough advance warning of approaching ovulation for those trying to prevent pregnancy.
- This study did not deliver any overly interesting data on Oura temperatures for menstrual cycle tracking, apart from showing that temperatures tended to be lower around ovulation, and then higher during the luteal phase (as expected). The study was not designed to test accuracy in comparison to oral temperatures and seemed to be more focused on sleep data.
 Device: BBRing by Femtek
Device: BBRing by FemtekPrice: First round on Kickstarter sold out, currently open to waitlist for next round of shipping. Price likely approx. USD $185
Type of skin temperatures (proximal or distal): Distal
Skin site: Worn in a ring to collect temperatures from the index finger.
Time worn: Only while sleeping
EMF exposure: The BBRing can be worn in “offline mode” overnight, reducing exposure to EMFs. Specific SAR levels are not provided, but the Femtek website states that "Our device has passed all EMC testing for the markets in which we are able to ship to, and due the ability to use the device in offline mode overnight, our EMF testers weren’t able to pick anything up on our readers."
Associated app: Basal Body Ring app
3rd Party integrations: Apple/Garmin health kit
Subscriptions required: No subscriptions required
Type of temperature data: Absolute values
Number of decimal places: Two decimal places (.00)
Data points provided:
- Temperature data
- Heart rate
- Heart rate variability
The BBRing has the potential to be a great addition to the FABM charting toolbox, because it will provide absolute temperature values to two decimal places. This means that the data provided will hopefully be comparable with Tempdrop, and you won’t need to do any calculations/conversions to get an absolute value for your chart (like you would if you were relying on the Oura Gen3 Ring or the Apple Watch).
Again, I don’t personally enjoy wearing jewellery so I would probably prefer the placement of the Tempdrop on the upper arm as opposed to a ring on my finger; however, I appreciate that this device only needs to be worn at night time.
I also like the fact that this device is made by a small Australian company who is prioritising menstrual cycle tracking – this is not simply another large multinational corporation adding on temperatures as an afterthought to try and capitalise on the femtech market. Olivia Orchowski (the founder), reached out to me in mid-2020 with questions on BBT for FABM charting. She was very responsive and open to feedback that would benefit the FABM charting community.
I’m excited to test out the BBRing myself. I am hopeful that it could hold the perfect mix of affordability, accuracy, and user-friendliness for FABM charting.
PS: Be sure to expand the Oura Gen3 Ring info section to read about some interesting study findings that may have applicability to the accuracy of the BBRing, too.
 Device: Apple Watch Series 8 / Apple Watch Ultra
Device: Apple Watch Series 8 / Apple Watch UltraPrice: From USD $390 / From USD $805
Type of skin temperatures (proximal or distal): Distal
Skin site: Worn on the left or right wrist (dorsal side) to collect wrist temperatures
Time worn: Can be worn continuously, or only overnight while sleeping if you are only wanting to use the Apple Watch for temperature tracking for charting.
EMF exposure: EMF levels for the Apple Watch Series 8 are not yet available on the Apple website; however, I can see that the Apple Watch Series 7 has a SAR level of 0.40 W/kg. This is significantly higher than the Oura Gen3 ring’s SAR level of 0.0003 W/kg.
Associated app: The iPhone Health App is used to access the nightly wrist temperatures. The Apple Cycle Tracking app is also available if you would like to make use of Apple’s period predictions. Unfortunately, Apple’s Cycle Tracking app doesn’t show a chart with enough detail to be used for FABM charting.
3rd Party integrations: There are a wide range of third-party apps that can be downloaded onto the Apple Watch. These include internet browsers, to sleep trackers, to heart activity trackers, to weather trackers, podcast players and so much more. Despite this, I am unaware of any 3rd party integrations that work with the Apple Watch temperatures for FABM charting.
Subscriptions required: No subscriptions required
Type of temperature data: Absolute temperature
Number of decimals: Two decimal places (.00)
Data points provided:
- Sleep data
- Temperature data
- Blood oxygen data
- Heart rate data
I like the fact that the Apple Watch does not need to be worn continuously, and it also does not require a subscription which is helpful given the rising costs of living. In addition, Apple provides temperatures with two decimal places.
The Apple Watch is not available to Android users, so is less accessible an option than some other femtech devices. It's also the most expensive wearable skin temperature tracking device that I investigated, which means it will be less accessible to those with less discretionary spending power
I don’t love wearing things on my hands/wrists at nighttime as I like to have my hands up near my face while I sleep, so I’m not sure whether this option would be suitable for me. I also am hesitant about the EMF levels which seem a little high in comparison with devices like the Tempdrop, Oura or BBRing.
At present, the Apple Watch Series 8 / Apple Watch Ultra doesn’t have much “social proof” for use with FABM charting, and therefore we don’t have much evidence as to how these temperatures might stack up against an oral/vaginal/rectal temperature chart.
So far, I have seen one chart comparing Apple Watch temperatures with oral temperatures, by charter Natalia Rodrìguez in the FAM Support Group Facebook group. The Apple Watch temperatures showed a slightly delayed temperature shift by only one extra day in comparison to oral temperatures; however, there were some missing oral temperatures around the time of ovulation so it is difficult to say how accurate this comparison is.
I think the Apple Watch Series 8 / Apple Watch Ultra may have potential for the future of FABM charting, provided that we begin to see some more evidence or social proof of the correlation between wrist temperatures and oral/vaginal/rectal temperatures. Importantly, there is some evidence that wrist temperatures may delay temperature shifts by around two days, and you can read more about that in the Ava Fertility Tracker bracelet section (again, it is not clear whether Ava studies would be relevant to Apple Watch Series 8, but we are working with the limited data we have at the moment!)
Studies (not an exhaustive list):
Ongoing: The Apple Womens Health Study in partnership with the Harvard School of Public Health. This study utilises data from Apple Watch users (with their consent), to investigate the “relationship between menstrual cycles, health, behavior, and habits.” I think this is a fantastic initiative considering that so much remains unknown when it comes to the intersection of our health and our reproductive hormones as women and/or people who menstruate.
Unfortunately, I cannot find any studies specific to the comparison of Apple Watch wrist temperatures to oral waking temperatures.
Note: I have found that the high levels of radio frequency emitted by the Apple Watch when communicating with my iPhone, interfere with the function of my oral BBT thermometer. I have heard the same for other smartwatches such as the Garmin. I recommend keeping all devices in airplane mode if you are using your BBT thermometer in the morning.
Expand the Ava Fertility Tracking bracelet section to read about some alternative studies on wrist temperatures and menstrual cycle tracking.
 Device: Ava Fertility Tracker bracelet
Device: Ava Fertility Tracker braceletPrice: From USD $280
Type of skin temperatures (proximal or distal): Distal
Skin site: Worn on the left or right wrist (dorsal side) to collect wrist temperatures
Time worn: Worn only while sleeping. Must be worn for at least 4 hours.
EMF exposure: It’s unclear from the Ava website whether the Ava Fertility Tracker emits EMFs while in use, and if so, what the associated SAR level is.
Associated app: Ava Fertility app
3rd Party integrations: None that I am currently aware of
Subscriptions required: No subscriptions required
Type of temperature data: Absolute values
Number of decimals: Two decimal places (.00)
Data points provided:
- Temperature data
- Heart rate
- Heart rate variability
- Breathing rate
I like Ava as a company because they have always been focused on assisting women and/or people who menstruate with fertility tracking for conception. I prefer this to companies such as Apple or Fitbit who add on menstrual tracking years after introducing their products. It says to me that Ava are wholly focused on us as a user base, as opposed to other companies who see menstrual trackers as simply a subset of their total userbase. I also love that they don’t require a subscription to be able to use their device.
I remain a little sceptical as to whether the Ava device has an acceptable sensor configuration and algorithm to provide accurate enough temperatures for FABM charting. Continue reading for my thoughts on a study that demonstrates this.
As with many of the other Femtech devices covered in this Info Hub, it seems the case that citizen science will need to come to the rescue if we really want to see accurate comparison charts through a FABM lens. Have you used the Ava bracelet and found that it provided accurate temperature readings in comparison to oral temperatures? Let us know in the comments below!
Studies (not an exhaustive list):
Shilaih M, Goodale BM, Falco L, Kübler F, De Clerck V, Leeners B. Modern fertility awareness methods: Wrist wearables capture the changes in temperature associated with the menstrual cycle. Biosci Rep. 2018;38(6):BSR20171279.
Goodale BM, Shilaih M, Falco L, Dammeier F, Hamvas G, Leeners B. Wearable sensors reveal menses-driven changes in physiology and enable prediction of the fertile window: Observational study. J Med Internet Res. 2019;21(4):e13404. doi:10.2196/13404.
Zhu TY, Rothenbühler M, Hamvas G, Hofmann A, Welter J, Kahr M, Kimmich N, Shilaih M, Leeners B. The Accuracy of Wrist Skin Temperature in Detecting Ovulation Compared to Basal Body Temperature: Prospective Comparative Diagnostic Accuracy Study. J Med Internet Res 2021;23(6):e20710.
- Study authors state that a cycle with a positive LH test was considered ovulatory; however, we know that in a small percentage of cases a positive LH test does not guarantee that ovulation will occur. Similarly, a cycle with only negative LH tests was considered anovulatory. Based on this criterion, 11% of cycles were deemed anovulatory.
- Temperature shifts occurred almost two days later with wrist temperatures when compared to oral temperatures.
- Study authors state that wrist temperatures rose to a larger extent (a mean of 11% higher) than oral temperatures in the luteal phase.
- Study authors state that wrist temperatures were more sensitive than oral temperatures, and therefore showed a “higher true-positive rate”; however, wrist temperatures were apparently more prone to showing “false positive” temperature shifts in cycles where no LH surge had been detected.
- My opinion after reading this study is that the Ava bracelet may be unsuitable for FABM charting. This is because temperature shifts will likely be delayed by approximately 2 days. In addition to this, Ava wrist temperatures are more sensitive and rise higher than oral temperatures in the luteal phase, which means that temperature shifts might be confirmed when oral temperatures would not be. Remember, Symptothermal Method rules have been established and studied based on oral/vaginal/rectal temperatures. It’s possible that these existing FABM rules may not be appropriate for the delayed/higher temperature curves created by the Ava bracelet. (Of course, it's also possible that these higher temperature shifts might be beneficial for some charters, especially those who have low progesterone and weak temperature shifts that are not well-served by existing FABM rules.)

Device: Fitbit devices (certain models/countries only)
Price: From USD $100 (Fitbit Inspire 3 which is a tracker) to USD $300 (Fitbit Sense 2 which is a smartwatch)
Type of skin temperatures (proximal or distal): Distal
Skin site: Worn on the left or right wrist (dorsal side) to collect skin temperatures
Time worn: Fitbit devices are designed to be worn continuously; however, I believe you can choose to wear them at night only if temperatures are all you are interested in.
EMF exposure: I have searched through the Fitbit website and cannot find details of whether Fitbit devices emit EMFs while in use, and if so what the associated SAR levels would be. There are numerous discussions of this topic on Fitbit community support boards, and moderators seem reluctant to disclose actual levels. Fitbit community board moderator "SilviaFitbit" says "The radiation emitted from all Fitbit devices is minimal. It is safe to use your tracker while pregnant.The Fitbit's power output is extremely low: about 0.5% - 1% of the output power of a cell phone. As for our Bluetooth-enabled devices, a good deal of research has been done in the field of Bluetooth radiation dangers to humans, and the general consensus is that the 800MHz to 2 GHz radiation output of a Bluetooth device is negligible".
Associated app: Fitbit app
3rd Party integrations: Fitbit devices are compatible with a wide range of 3rd party apps such as Strava, Peloton, Mindbody, Lumosity, MyFitnessPal and more. Despite this, I am unaware of any 3rd party FABM apps that can harness Fitbit skin temperatures for charting.
Subscriptions required: You can access your average nightly skin temperatures without a premium subscription; however, if you would like to see the full fluctuation of your temperatures through the night, you will need a premium subscription. A premium subscription costs US $9.99 per month.
Type of temperature data: Like the Oura Gen3 Ring and the Apple Watch Series 8/Ultra, Fitbit devices provide skin temperature changes as fluctuations (+/-) from your personal “baseline temperature”. Fitbit calculates your baseline temperature based on up to 30 nights’ worth of previous temperatures. Fluctuation trend data is less useful for FABM charting, as we need actual temperature values to plot on the graph section of our charts each morning. The Fitbit website states that temperature information is not available in all markets.
Number of decimal places: One decimal place (.0)
Data points provided:
- Resting heart rate
- Sleep data
- Oxygen saturation
- Temperatures
I like that the Fitbit Inspire 3 (at approximately USD $100) is the most affordable wearable skin temperature tracker on this list, meaning it will be accessible to a wider range of people. In addition, a premium subscription is not required to access daily temperature information.
I don’t really like to wear rings or watches to bed, because I keep my hands up by my head while I sleep and I find that jewellery on my fingers/hands interferes with my sleep. That said, the Fitbit Inspire 3 is a much more slimline design in comparison with the Apple watches, which is a drawcard for me.
Unfortunately, just like the Oura Gen3 Ring and the Apple Watch Series 8 / Ultra, the Fitbit app only provides users with fluctuation trends when it comes to daily temperatures. This means that the Fitbit lacks any “social proof” for use with FABM charting because it doesn’t provide actual temperatures which can be used on a chart.
I have personally tested the Fitbit Inspire 3 band and it provided extremely erratic temperatures that were wildly inaccurate on my chart (using the formula further down this page to obtain actual temperatures from the Fitbit fluctuation trends). Due to this, I do not recommend anyone spend money on this device to use for FABM charting.
Studies:
Expand the Ava Fertility Tracking bracelet section to read about some studies on wrist temperatures and menstrual cycle tracking that may have relevance for Fitbit devices.
If you’ve read this far, you’ve now learned how different types of temperatures differ across 24hr and infradian menstrual cycles, and how this might impact FABM charting. You’ve also learned more about the features, pros and cons of some of the main wearable skin temperature trackers available on the market today.
But what about some of the more common frequently asked questions? Expand each of the headlines below to learn more about how to get absolute temperatures, whether your device displays enough decimals for FABM charting, how accurate your sleep data is, how the placebo and nocebo effect might impact you, and more.
Finally, how does using a wearable skin-temperature tracker impact the effectiveness of your chosen Fertility Awareness Based Method? This is arguably the most important question that this entire article addresses, so please take the time to read this section thoroughly.
![]()
With the Oura Gen3 Ring, you do have the option of downloading the Natural Cycles app to be able to see your absolute temperatures; however, a lot of Symptothermal Method charters prefer not to use Natural Cycles app.
Is it too much to hope that these devices might provide absolute temperature values in future? I have read some opinions on the internet that the reason these devices don’t offer absolute temperatures, is that it is too easy for people to compare them against oral/other temperatures and then worry that perhaps the devices are not as accurate as they would have hoped.
Thankfully, FABM charters don’t generally need our temperatures to be perfectly “accurate”. Instead, what we are looking for is precision. We are looking at the overall pattern of our chart to identify temperature shifts. It doesn’t matter whether temperatures are slightly “out” by a certain amount, just so long as that error is consistent across every day of the whole menstrual cycle.
Accuracy: How close a measurement is to the true value.
Precision: How consistent results are when measurements are repeated.
If you have your heart set on using a wearable device like the Oura Gen3 Ring or a Fitbit you will need to find a way to extract absolute temperature values to use on your chart. It's possible that you might be able to do this by assigning a random temperature reading as your “baseline temperature”. As an example, I would assign 36.5°C as a random baseline. Each day, my device will provide me with a figure for how much my temperature has deviated from the official baseline. I would then need to either add or subtract this figure from 36.5°C to provide an absolute temperature value for that day.
For example, if your Oura ring tells you that your temperature is “-0.3°C” you would subtract 0.3 from 36.5 for today’s temperature value of 36.2°C. Alternatively, if your Oura ring tells you that your temperature is “+0.6”, you would add 0.6 to 36.5 for today’s temperature value of 37.1°C.
In this way, you will be able to plot temperature values on your FABM chart. Remember, we don’t need temperatures to be perfectly accurate, we simply need them to be measured consistently each day so that we can identify the temperature shift caused by ovulation.
There are two caveats to this approach.
The first is that it’s possible that your device may update your “personal baseline” temperature without letting you know (in fact, Fitbit directly states on their website that your personal baseline is based on a rolling average calculation of your 30 most recent nights of data). I am imagining that changes to your "personal baseline" could occur for many different reasons over the span of several weeks or months. For example, you stop/start a new thyroid medication (which can impact core temperatures). Alternatively an effect might be seen if you implemented lifestyle changes (for example fasting/increased caloric intake/increased energy output/decreased energy output) that can impact your metabolism and core temperature. I am of the opinion that it is very likely that this could occur, and if so it will impact the precision of all subsequent temperatures on that particular chart.
Secondly, even with manual calculation of daily temperatures based on fluctuations from your personal baseline, Oura and Fitbit Celsius charters may still be lacking a second decimal place. Read on for more information on how the number of decimal places can impact FABM charting.
Finally, remember that you will be operating well outside of “perfect use parameters” if you decide to take this approach to obtain temperatures for your Symptothermal Method chart. Read on to learn more about effectiveness estimates.
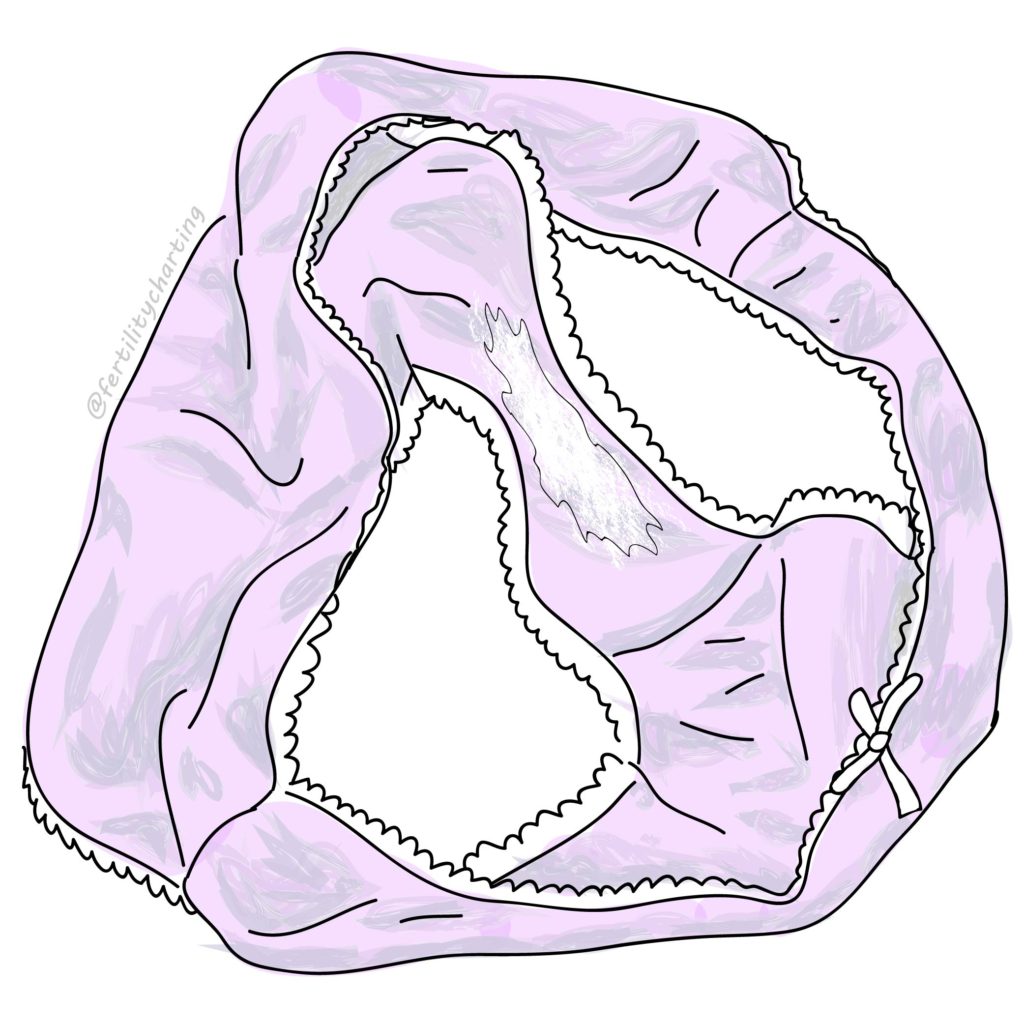
When it comes to charting your temperatures, you will plot rounded temperatures on the graph section of your chart. Most Symptothermal Methods require that you round your raw temperatures to the nearest 0.05°C/0.1°F (Fahrenheit charters will use scientific rounding, while Celsius charters use a slightly different rounding technique).
Does your device display your daily temperature to two decimal places? It may be that your wearable device has been proven to take highly accurate temperatures in clinical settings, but when it comes to the public app interface, they are only sharing a single decimal place with you.
This specific situation is an issue for Celsius charters, who need to be able to chart to the nearest 0.05°C, which is not possible if your device only displays a single decimal digit.
So, always take information based on BMI with a grain of salt, and consider whether the information may/may not apply to you personally.
If you have a higher BMI, I have heard anecdotal stories from other Symptothermal Method charters who have struggled to gain accurate skin temperatures using devices such as the Tempdrop, and believe it may be due to their weight. I’ve heard this from around 3 separate people at this point (not a huge number, but enough to pique my interest!).
Interestingly, there may be some truth to their suspicions regarding BMI and skin temperatures. A 2019 study titled ‘Nocturnal finger skin temperature in menstrual cycle tracking: ambulatory pilot study using a wearable Oura ring’ found that the accuracy of the Oura algorithm increased when the two study subjects with a BMI of over 30 were excluded from the calculations. Study authors state that a BMI of over 30 “is a potential confounder affecting distal skin temperature.”
A 2009 study titled ‘Adiposity and human regional body temperature’ showed that obesity causes distal temperatures to rise, to account for the insulating effect of a greater layer of subcutaneous abdominal fat. These higher distal temperatures allowed study participants to release heat and therefore regulate their core body temperature.
Is it possible that a higher baseline distal temperature might mute the post-ovulatory rise in distal temperatures, and therefore make it difficult to identify an accurate temperature shift? I would love to see more studies on this in future (for both distal and proximal temperatures), and in the meantime it is something that those with a higher BMI may want to keep in mind.
Usually, sleep studies are performed under laboratory conditions using an assessment technique known as polysomnography. According to the Mayo Clinic, “polysomnography records your brain waves, the oxygen level in your blood, heart rate and breathing, as well as eye and leg movements during the study.”
Because wearable devices are currently limited to far less data points than are available in clinical sleep studies, it’s no surprise that accuracy may be lacking.
For example, Oura’s own website states that their sleep data only agrees with laboratory polysomnography results 79% of the time!
Additionally, a 2021 study tracked the accuracy of eight separate wearables/associated sleep analysis apps (Apple Watch Series 3, Beddit Sleep Monitor 3.0, Fatigue Science Readiband, Fitbit Ionic, Garmin Vivosmart 4, 2nd generation Oura smart ring, Polar A370, and the WHOOP Strap 2.0). The study found consistent trends across all devices showing failure to accurately determine the amount of time that the wearer was awake as opposed to asleep. Interestingly, the Oura and Fitbit were found to be the most accurate of these studied devices/apps.
These results may be because it is very difficult for wearable devices to differentiate between when you are simply laying quietly in bed with a lowered heart rate trying to fall asleep, versus when you actually are asleep. This can result in overestimation of the total sleep time.
Have you ever woken up feeling great, but then check your wearable sleep data to see that you barely got any deep sleep the night prior, and you suddenly feel a bit more tired?
Alternatively, do you ever wake up exhausted, but then check your Oura App to see a high “readiness score”, and suddenly pep up a little bit?
I think it’s important to be cognisant of the way that femtech can impact our daily experiences in this way, especially if the sleep data that we are receiving is inaccurate.
There’s a lot to say for simply waking up and listening to what your body is telling you (as opposed to what an app is telling you about your body).
If you are someone who struggles with the effects of information overload in our digital landscape, consider opting for a tried-and-true oral basal body temperature thermometer instead. This can be a breath of fresh air for many people. Remember, you know yourself best; if this is the case you can usually find an affordable $20 thermometer from your local pharmacy (and you can find a list of recommended BBT thermometers here).
Not only will you enjoy some respite from the onslaught of digital information, but you will be able to rest easy knowing that oral/vaginal/rectal temperatures are the only ones that have been proven safe and effective for FABM charting in clinical trials.
You’re operating closer to perfect use parameters if you choose a standard BBT thermometer over a wearable skin-temperature tracker.
To meet perfect-use parameters for the Symptothermal Method you need to be relying on oral, vaginal or rectal temperatures. Other temperature collection sites have not been assessed in clinical trials for accuracy when used as a part of the Symptothermal Method.
This means that if you choose to rely on any wearable skin temperature collection device (including the popular Tempdrop), you are now operating outside of perfect use parameters and heading more toward typical use effectiveness rates (although by exactly how much, it is difficult to say).
Depending on how seriously you are needing to prevent a pregnancy, this may or may not be acceptable to you and your partner. This is a situation where you need to be clear on your reproductive intentions and your specific situation.
If it’s important to you to continue using a Symptothermal Method and attain BBT readings closer to your actual core temperatures, consider investigating internal temperature wearables. These include devices such as Ovolane, Trackle, OvuSense and iButton. Many of these are more popular in European markets.
Given that the Tempdrop smart thermometer has a large user base of well over 10,000 users, and has been in use within the FABM community since 2017, many people (myself included) generally have a good level of trust in the accuracy of temperatures provided. I personally use the Tempdrop myself and am satisfied with the charts I receive; it has made postpartum charting a breeze for me. Not everyone shares this good experience though; in fact some charters report that they have struggled to get accurate readings with their Tempdrop. You can read more about the pros and cons of the Tempdrop here. Other wearable skin temperature trackers do not yet share the same social proof for FABM charting that the Tempdrop does.
My recommendation is that if you wish to rely on skin temperatures (from any wearable device!) for use with your chosen FABM, you should spend at least the first three menstrual cycles’ of use comparing your skin temperatures against your oral, vaginal or rectal temperatures. Even after confirming that the temperatures follow the same pattern and you are able to confirm temperature shifts on (or around) the same day, it’s still important to note that you are still operating outside of perfect use parameters. Ensuring you are cross-checking against cervical mucus with a Symptothermal Method likely adds some safety, but is still outside of perfect use parameters. If you're seriously trying to avoid pregnancy, I definitely would not recommend using skin temperatures with a "temperature-only FABM" (such as Natural Cycles).
In saying all of the above, I encourage everyone to experiment … for science! If experimenting with different forms of femtech means you find ways to make your chosen FABM more accessible and convenient – more power to you. Convenience usually means that you are more easily able to stay compliant with the data collection requirements of your FABM, which is beneficial for effectiveness.
So, the bottom line is (as always), you do U-terus. As long as you are making informed decisions based on accurate information, you’re on the right track.
Have you found this Info Hub helpful? Do you have any thoughts to add? Let me know in the comments below; I love hearing what others think about the latest FABM topics.
![]()