Not a month goes by where I don’t get a question or a comment along the lines of “I’ve heard that you can spontaneously ovulate when the moon is in the same phase as it was when you were born… is that true?” As it seems there are a lot of people wondering the same thing, let’s dive into the research!
NATAL LUNAR CYCLES
To answer the question of whether the moon causes random ovulation, it’s helpful to establish where this concept originated. In fact, it all stems from a method known as “Natal Lunar Cycles” created in 1956 by Dr. Eugen Jonas, a psychiatrist from Slovakia. Dr. Jonas was a devout Catholic. When laws legalising abortion were passed in nearby Hungary in 1956, he decided to investigate whether there was a way to help women avoid unplanned pregnancies (and therefore the need for abortion). Throughout much of history, humans have connected the moon with female fertility due to the similarity of their cycles (the textbook menstrual cycle is 28 days long, and it takes around 29.5 days for the moon to orbit the earth). Dr. Jonas gravitated toward this theme in his search for answers.
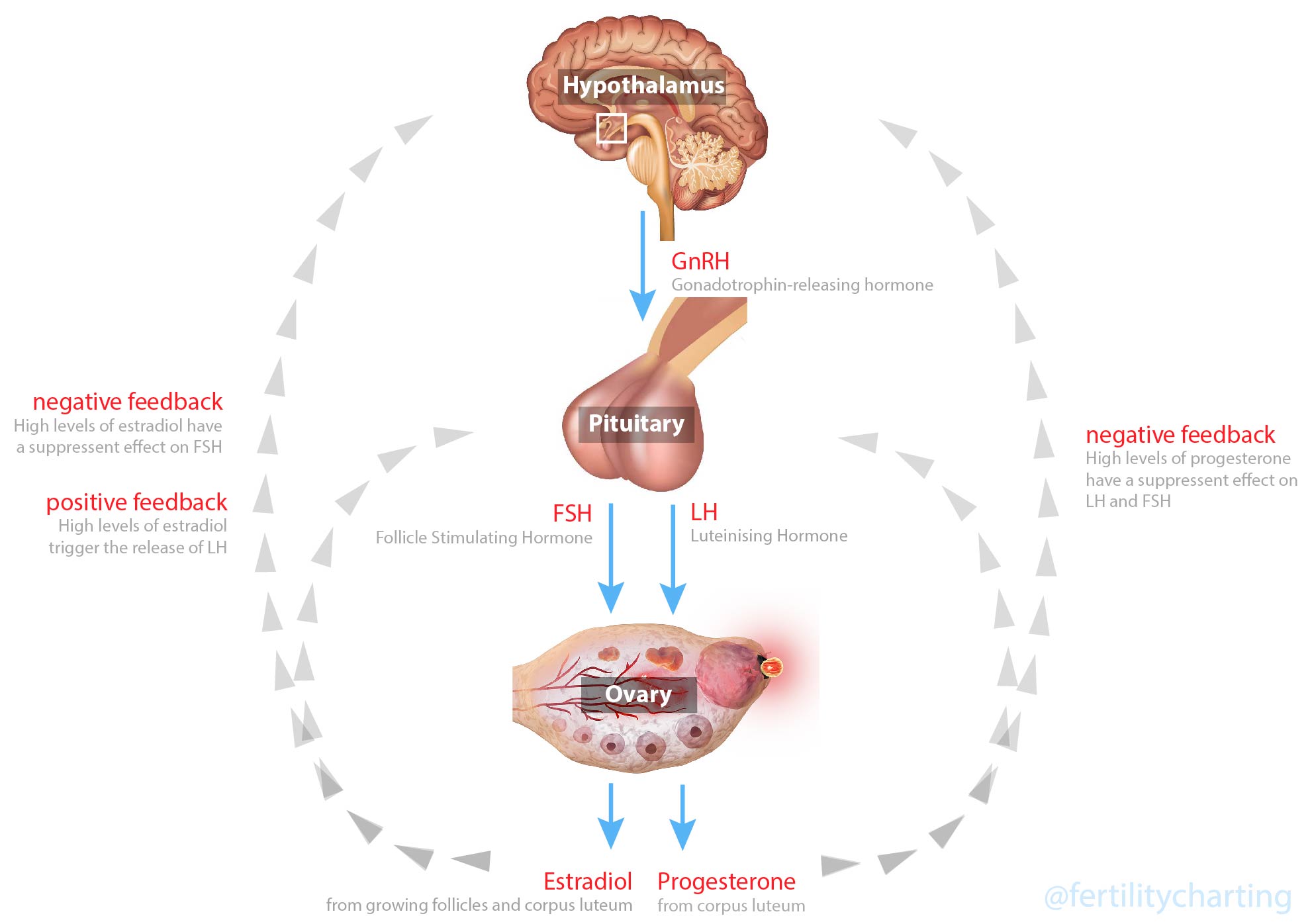
Dr. Jonas formulated a theory that women had two separate fertility cycles:
- The usual and expected ovulation cycle (ovulation occurring roughly in the middle of the menstrual cycle), and
- A lunar cycle
Jonas theorised that women could ovulate at spontaneous times outside of their usual time of ovulation, and this was likely to occur when the moon was in the same phase as it was at their birth. For example, if you were born two days before a waning crescent moon, then you could expect to always be highly fertile two days before the waning crescent moon (regardless of where that might fall in your current menstrual cycle).
Calculations were done in advance to identify where these “lunar fertile” days would fall throughout the year. Dr. Jonas would then advise his patients to abstain from sex for at least four days around this time. Usually, it was specified to avoid the three days leading up to the “lunar fertile” day, and the “lunar fertile” day itself, as well as a full 13 days identified by the Rhythm Method. This totalled at least 17 days of abstinence out of every menstrual cycle!
Jonas also developed calculations that were supposed to assist with gender selection and avoiding foetal abnormalities.
Dr. Jonas claimed his method (combining lunar fertile days with the Rhythm Method) showed a 97.8% effectiveness (although I can’t find any record of the studies that are supposed to support these findings anywhere online).

WHAT IS THE RHYTHM METHOD?
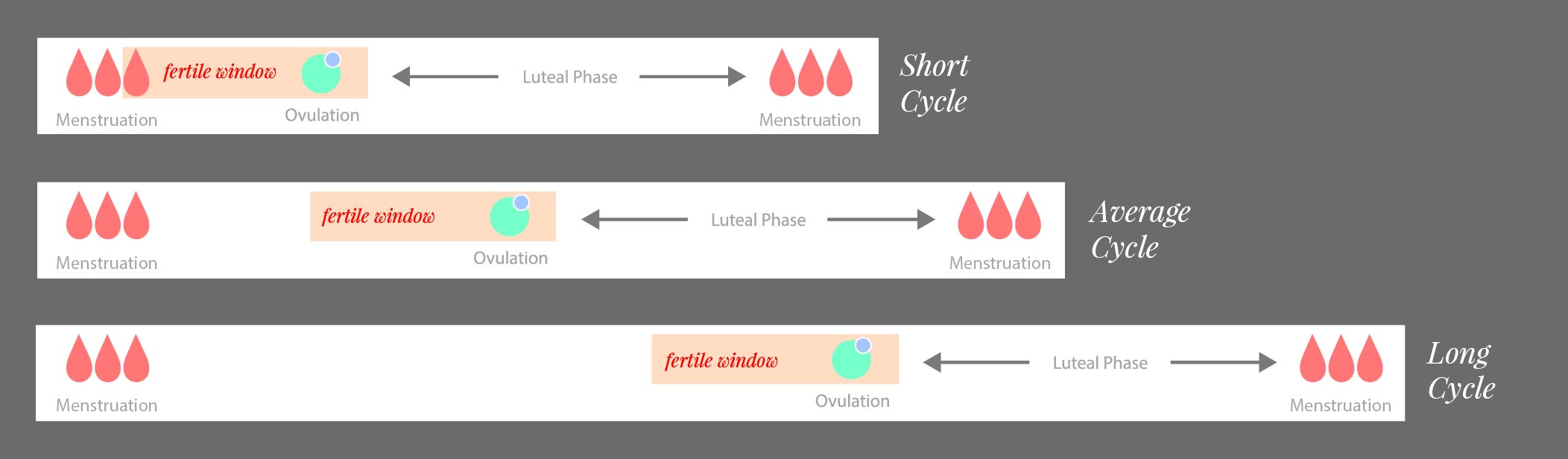
To really understand Dr. Jonas’ method, it’s important to understand the Rhythm Method. The Rhythm Method is an outdated relic of the 1930s, where women predict their fertile days based on the lengths of their previous 12 menstrual cycles. The Rhythm Method has only low-quality scientific studies to support it, and an estimated effectiveness rate of around 80% which is generally unacceptable by today’s standards. The Rhythm Method assumes that every woman will ovulate approximately 14 days before her next period, every menstrual cycle. This assumption (and the lengths of your previous 12 cycles) is used to determine when you should avoid unprotected sex.
Why is it so ineffective? In a nutshell, humans are not robots: there is wide variation among women, and even for the same woman when it comes to our menstrual cycles. Many of us have a luteal phase that is significantly shorter or longer than the 14 days assumed by the Rhythm Method, and many things can cause us to ovulate earlier or later than we have in the past 12 months.
As it turns out, Dr. Jonas’ method doesn’t actually follow Rhythm Method rules, but it does apply “rhythm method thinking” by assuming that every woman will ovulate on day 15 of her menstrual cycle. Jonas’ method states that the user must abstain from sex for a full 13 days around this assumed day of ovulation: “Starting from this ovulation day [cycle day 15], add six days before and six days after this ovulation day.”
When combined with the four days of abstinence required around the “lunar fertile” day, that’s a total of 17 days of abstinence required each menstrual cycle!
It’s no surprise that Dr. Jonas had some level of success with his method when you consider the sheer number of days that his users were having to abstain from unprotected sex.
HISTORICAL CONTEXT
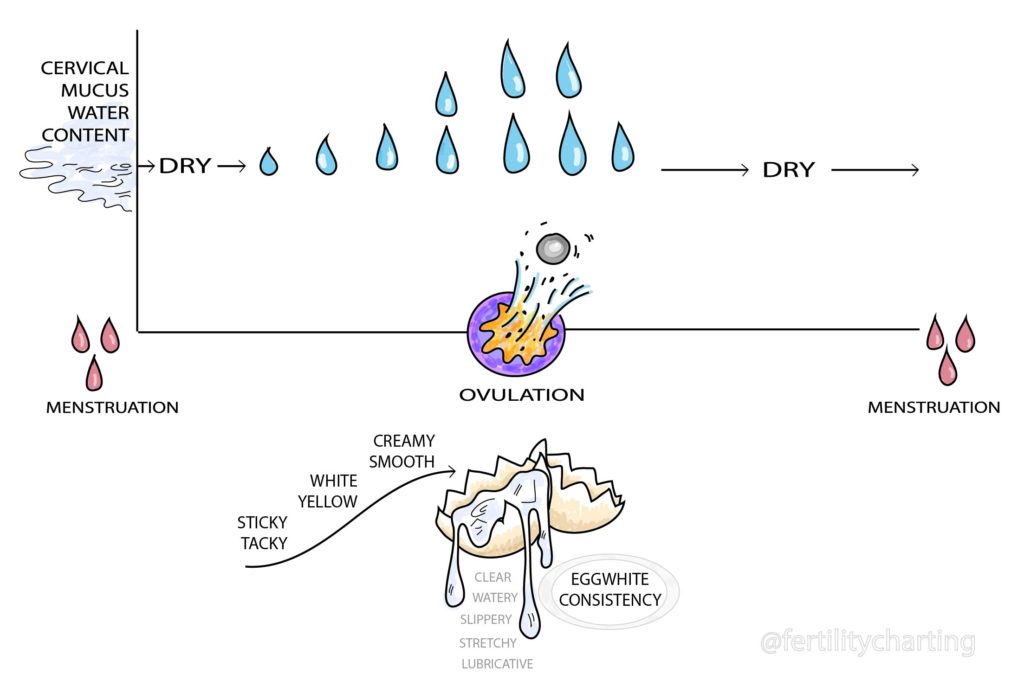
Dr. Jonas developed his method in 1956 at a time when the importance of cervical mucus was only just being realised by the medical establishment. Cervical mucus provides real-time insights into our hormones because it changes in sensation, colour, amount and texture in response to our hormones. You can read more about cervical mucus here. The value of basal body temperature in confirming ovulation had already been known since the 1930s so it’s unclear why Dr. Jonas didn’t utilise this information. Instead, in a rather bizarre choice for a Catholic, Jonas decided to pursue the field of astrology for answers to a question that would have been better served by biology.
The Symptothermal Method itself was officially born in 1953 when Dr. Edward F Keefe added daily mucus observations to the existing Calculo-Thermal Method. With the spread of knowledge around cervical mucus, methods such as the Rhythm Method gradually lost favour as practitioners realised that we could monitor our fertility in real-time (as opposed to making “best-guess” predictions that left us open to error).
THESE DAYS
Thankfully, we now have very solid evidence of the way our reproductive biology functions each menstrual cycle and are no longer at the mercy of haphazard lunar predictions or the ineffective Rhythm Method. The myth of multiple ovulation is well and truly de-bunked ((you can read about that here). Plus, we have a fantastic longitudinal European study that established a 99.6% perfect use effectiveness rate for the Symptothermal Method.
This 99.6% effectiveness rate would have been completely unattainable if Dr. Jonas’ theory had a single shred of credibility.
In fact, in the entire 20 years of this longitudinal prospective clinical trial, not a single method error pregnancy was ever recorded during the luteal phase after ovulation had been confirmed by Symptothermal Method rules.
BUT WHAT ABOUT SUCCESS STORIES?
For the Symptothermal Method charter, it can be very frustrating to hear anecdotes along the lines of “I know I ovulated on the Friday, and we had sex the following Thursday and ended up pregnant – I know for certain that I ovulated twice!”
In these cases, I always say “Interesting! Can you show me your chart?”. I have never once had anyone show me a chart.
Invariably, most people with stories like this were not charting with any reliable method but simply noticed some “ovulation pain” or saw a positive OPK test and assumed that this meant they had definitely ovulated. [Hot tip: Neither mittelschmerz nor a positive OPK test are a guarantee of ovulation].
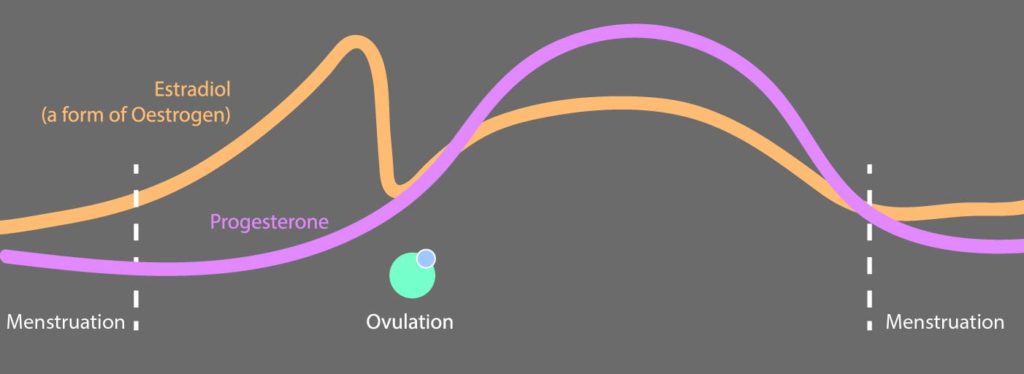
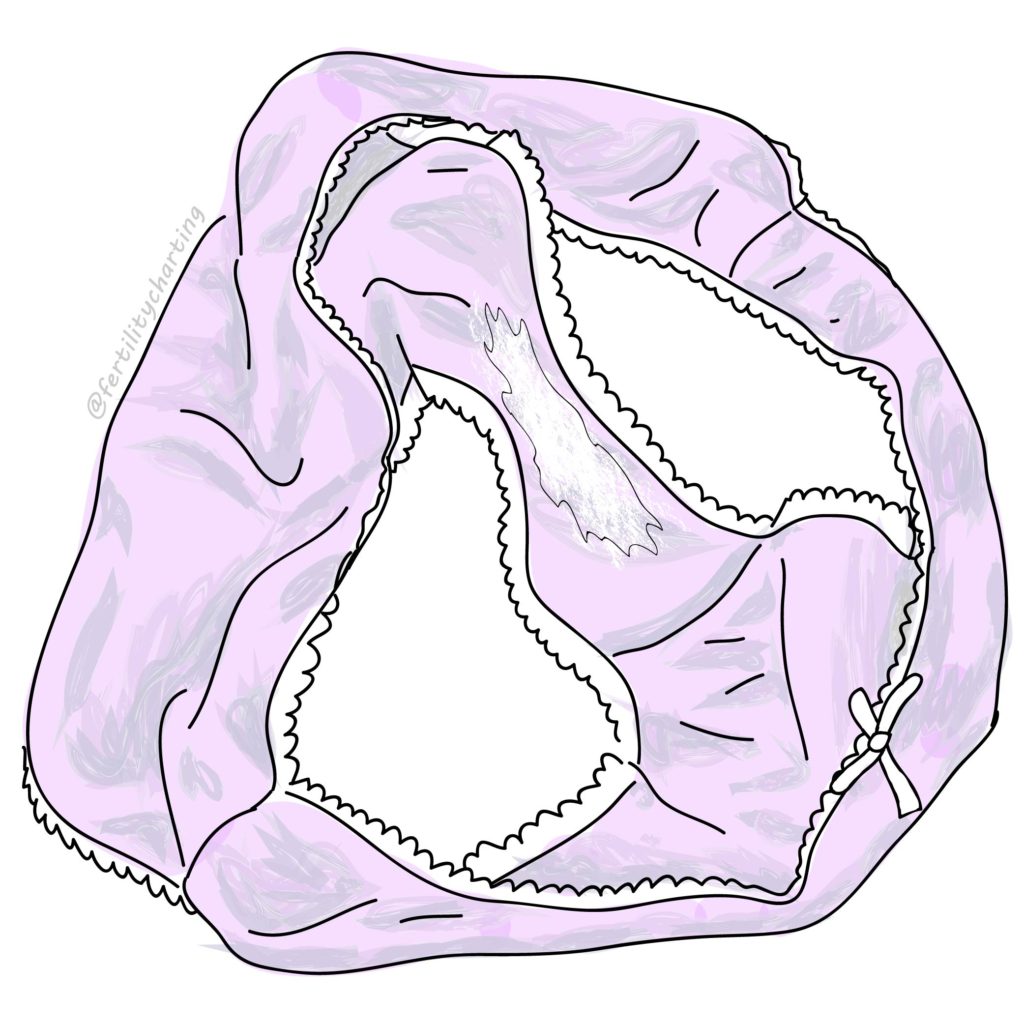
In other cases, the woman was relying on mucus observations alone and assumed that seeing eggwhite cervical mucus guaranteed that ovulation was occurring. [Hot tip: highly fertile peak type mucus is an indicator of high oestrogen levels – however this does not guarantee that ovulation will occur].
Without a chart which shows a sustained temperature rise and a dry-up of cervical mucus that meets the specific rules of the Symptothermal Method, these anecdotes prove nothing (except that the person telling them does not have a sufficient understanding of their cycle to make any claims about multiple ovulation).
IN REAL LIFE
As a seasoned charter and a certified Symptothermal Method instructor, I’ve actually put Dr. Jonas’ theory to the test myself. I sent my beautiful mother a Facebook message and asked her to dig out my birth certificate and confirm for me the exact time of my birth, 30 years ago! (Wow, time flies!). I used a simple calculator available freely on the internet to find out my “lunar fertile” days and then I compared them to my past 12 menstrual cycle charts.
What do you know? The majority of those supposedly highly fertile days fell firmly in my menstrual or luteal phases – and I can tell you I’ve had plenty of unprotected sex during those times that definitely have not resulted in a pregnancy. (Please keep in mind that it is possible to conceive from period sex. These were the times specific to my own unique cycle that were identified as safe days using the Symptothermal Method.)
Are you a seasoned Symptothermal Method charter and feeling curious? You can try it here to debunk this myth for yourself: https://horoscopes.astro-seek.com/calculate-pregnancy-fertility-days/
Mostly, this experiment made me feel sad when I thought of the women who may have tried to do the same thing by actually paying Jonas. He has multiple websites that all seem to offer different services, one of which is providing dates of “good vitality” for women who have suffered miscarriages and foetal abnormalities. This comes in at a cost of around AUD $80 and stinks of predatory behaviour.
BUT WHAT ABOUT THE ~TIMING~ OF OVULATION?
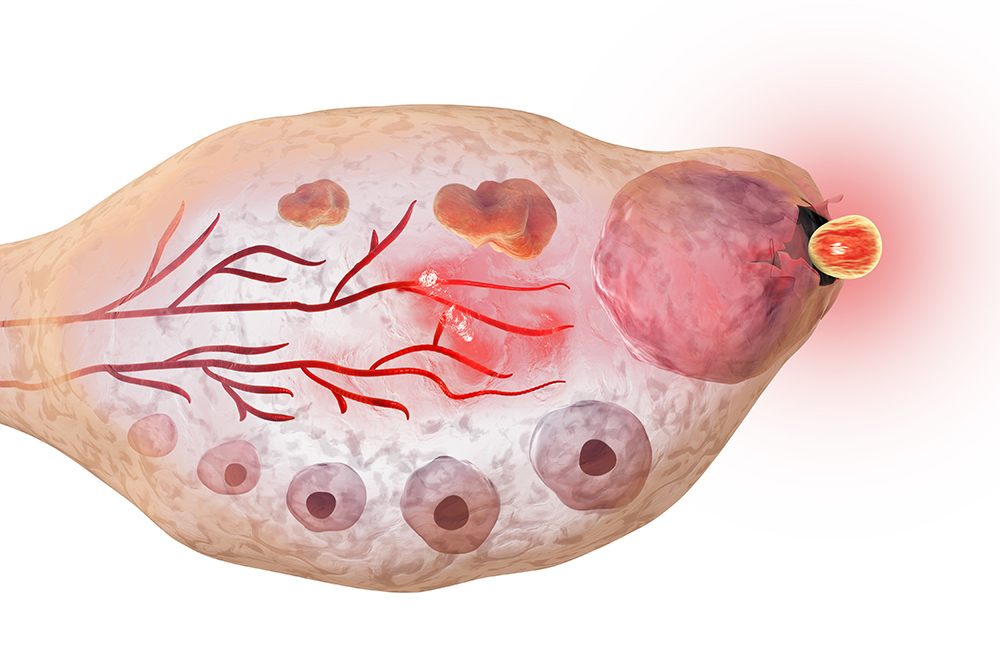
While the moon cannot cause you to experience two ovulations in a single menstrual cycle, there is some evidence that the luminescence and gravimetric cycles of the moon may influence the timing of menstruation (and therefore ovulation).
A 2021 study looked at data from 22 women, who had each recorded period onset dates for an average of around 15 years. The researchers found that menstruation occurred more often around the new moon and full moon than would be expected to occur by chance.
Luminescence (light) appeared to impact the timing of ovulation for some women, some of the time.
The same was found for apogee and perigee dates, when the moon is closest to or farthest from earth and exerting maximal or minimal gravitational force.
These impacts were temporary, meaning menstruation start dates would cluster around new moon/full moon and apogee/perigee dates for some time, before drifting away again. However, this was occurring more often than would be expected to occur due to chance.
The researchers hypothesise that human reproductive behaviour may have been syncronous with the moon in ancient times. They also hypothesise that our modern lifestyle and increasing exposure to artificial light may now be inhibiting the display of these ancient menstrual onset patterns.
CONCLUSION
There’s much we don’t know in this world, and science certainly does not have all the answers. There is definitely some interesting research out there about the impact of light on our fertility! However, if Natal Lunar Cycles were a valid hypothesis then the Symptothermal Method would be vastly less effective than it has been proven.
The verdict? The moon will not cause you to spontaneously ovulate. Natal Lunar Cycles is a now-outdated theory that will only result in unnecessary abstinence on your part (or unfounded hope if you are trying to conceive).
Jess x