Disclaimer: I am writing this article from the depths of postpartum sleep deprivation. Please also keep in mind that I am not qualified or trained to interpret contraceptive effectiveness estimate research papers so I encourage you to read the latest systematic review for yourself to form your own opinions about FABM charting in the postpartum 😊
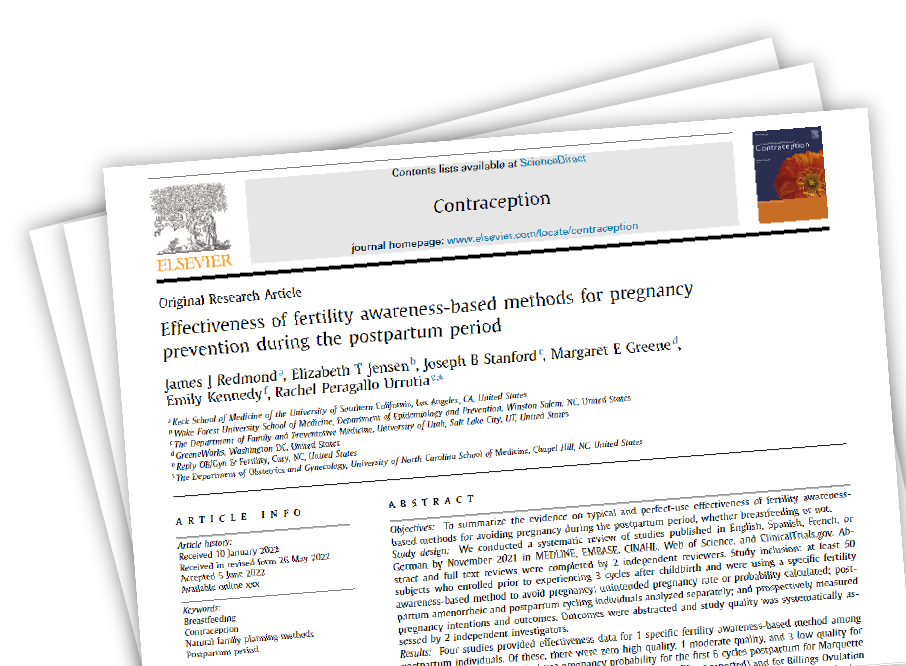
Last month (in June 2022), a new systematic review was published titled ‘Effectiveness of fertility awareness-based methods for pregnancy prevention during the postpartum period’. You may remember a previous systematic review that was published back in 2018 titled ‘Effectiveness of Fertility Awareness–Based Methods for Pregnancy Prevention’ – well, four of the authors of that 2018 review were also involved in this most recent systematic review. Those four authors are Rachel Peragallo Urrutia, Margaret E Greene, Emily Kennedy and Joseph Stanford.
I was made aware of this latest systematic review after Dr. Chelsea B. Polis shared a link to it in the popular Facebook group ‘Fertility Awareness Method of Birth Control’. Dr. Polis was one of the authors of the original 2018 systematic review, and is also known for having fought for the publics’ right to accurate information about the effectiveness of the Daysy fertility monitoring device. You can read more about this story by visiting this Instagram highlight.
Being currently postpartum myself, I was interested to read the latest systematic review for an updated perspective on the use of FABMs during this unique reproductive life phase.
For those not familiar with the postpartum period, the return of fertility after birth can be highly variable among different people, and is significantly affected by breastfeeding. The first postpartum bleed may or may not be preceded by ovulation, and it is not possible to predict when ovulation will first occur. The body may attempt multiple times over many months to ovulate, and once ovulation does return, cycles may remain irregular for some time. Breastfeeding can also contribute to erratic temperatures and changed cervical mucus patterns. All of these factors combine to create conditions that render FABMs difficult to apply to the postpartum. You can read in more detail about the hormonal and physical landscape of postpartum in relation to FABMs in this article: https://fertilitycharting.com.au/2019/03/31/postpartum-fertility-i-just-had-a-baby-now-what/
A little about my postpartum experience:
I gave birth to Sol in December 2021, and originally planned to learn the Billings Ovulation Method (B.O.M.) while in “Cycle 0”. Cycle 0 is the time from birth up until your first ovulation and true menstruation. For FABM users who are fully breastfeeding, cycle 0 can span many months (even over a year!). While the Symptothermal Method really shines for those in relatively regular cycles during times of regular fertility; it tends to have basic mucus protocols that sometimes lack some of the necessary nuance for the postpartum cycle 0. For this reason, I hoped to learn a cervical mucus-only type of FABM, and had my sights set on the B.O.M.

What I hadn’t factored in was the absolute intensity of the newborn phase with a colicky baby, a partner working 6 days a week, international travel restrictions keeping me separated from my family support system, a hefty dose of Covid sickness, a one-woman small business to keep afloat, and ongoing pain due to breastfeeding-induced Reynaud’s phenomenon of the nipple. It’s safe to say that learning the B.O.M. rapidly dropped completely off my to-do list.
Not to mention sex dropped rapidly off my to-do list, too!
In addition to this, most Symptothermal Methods only have postpartum protocols designed to accommodate simple “basic infertile patterns” of either continuing dryness, or continuing scant white mucus. My breastfeeding basic infertile pattern did not match either of these. This meant that if I didn’t learn the B.O.M., then I couldn’t even fall back on using the Symptothermal Method during cycle 0.
With all that said, my approach to charting in cycle 0 was to utilise what is known as coitus dependent contraception – contraceptive methods that are employed at each sex act to reduce the risk of pregnancy. So, this means things like barrier methods in combination with withdrawal. There are ways to maximise the safety and effectiveness of coitus-dependent contraceptives (and I teach this to clients in the Natural Contraception online course). Given the fact that ovulation returned for me relatively quickly (just over 3 months after having given birth), I didn’t mind utilising coitus-dependent contraceptives during this time.
After ovulation returned, I have been utilising coitus-dependent contraceptives during both Phase 1 and Phase 2 of my menstrual cycle, with unprotected sex reserved for Phase 3 only. This is due both to my reproductive intentions, and also because my charting practise remains a little sparse and ad hoc while I lack time and energy. Haphazard charting can put you at risk of missing the transition from Phase 1 to Phase 2 of the menstrual cycle, and for this reason I am currently choosing to utilise Phase 3 only. If the terms ‘Phase 1’, ‘Phase 2’ and ‘Phase 3’ are new to you – this is terminology which I teach clients in the Natural Contraception online course and is used to denote the infertile-fertile-infertile transition identified by the Symptothermal Method during regular ovulatory menstrual cycles.
Although I was personally too overwhelmed to learn a new FABM during the immediate postpartum, I was curious to delve into this systematic review. From my personal experience, I feel as though the postpartum time remains an underserved timespan of the reproductive life phases, and I was curious as to what the authors found on this subject.
Some key points from the systematic review:
So what did the systematic review find? Some key points are below. I also encourage you to read the systematic review for yourself, and you can find it here (although it is behind a paywall): https://www.sciencedirect.com/science/article/pii/S0010782422001573?dgcid=author
- There is a decided lack of evidence for the effectiveness of FABMs in the postpartum. The systematic review authors state that “The current evidence on the effectiveness of each fertility awareness-based method for postpartum persons is very limited.” Given the fact that in Australia, over 84% of women aged 45-49 have already given birth1, it is a shame that we lack evidence on the use of FABMs during this very common reproductive life stage.
- The systematic review authors searched huge databases of thousands of studies against a very strict inclusion criteria to ensure that they would only be assessing studies that accurately appraised the effectiveness of FABMs in the postpartum. Because of the strictness of this inclusion criteria, they were only able to assess four studies.
- Of these four studies, three were deemed of low quality and one was deemed of moderate quality.
- The Symptothermal Method (which I use and teach) was not included in the systematic review as no studies met the inclusion criteria. The 2007 Sensiplan study which is most often quoted by users of Symptothermal Methods could not be included because it did not meet all of the study inclusion criteria: “at least 50 subjects who enrolled prior to experiencing 3 cycles after childbirth and were using a specific fertility awareness-based method to avoid pregnancy; unintended pregnancy rate or probability calculated; postpartum amenorrheic and postpartum cycling individuals analyzed separately; and prospectively measured pregnancy intentions and outcomes”.
- The studies that were included showed a range of effectiveness rates that may or may not be acceptable to different individuals, depending on their reproductive intentions (how seriously they are needing to prevent a pregnancy).
Marquette Method, Bouchard 2012, United States, low quality study:
o Typical use effectiveness per cycle during the first 6 cycles postpartum:
88%
o Perfect use effectiveness per cycle during the first 6 cycles postpartum:
98%
(additional effectiveness estimates for different time frames are available in the systematic review)
Billings Ovulation Method, Labbok 1991, Kenya, low quality study:
o Typical use effectiveness during the first 12 months postpartum:
81.5%
o Perfect use effectiveness during the first 12 months postpartum:
85.9%
(additional effectiveness estimates for different time frames are available in the systematic review)
Billings Ovulation Method, Perez 1988, Chile, low quality study:
o Typical use effectiveness during the first 12 months postpartum:
88.9%
o Perfect use not provided
(additional effectiveness estimates for different time frames are available in the systematic review)
Bridge to Standard Days Method, Sinai 2012, Peru, Guatemala, moderate quality study:
o Typical use effectiveness during the 6 months after the first postpartum bleed:
88.2%
o Perfect use effectiveness during the 6 months after the first postpartum bleed (including use of condoms):
96.3%
- The authors emphasise that the above individual FABM effectiveness rates cannot be directly compared to one another. This is because the studies themselves were all quite different, of relatively low quality, and the effectiveness estimates are for different postpartum timeframes.
- Individual study results may not be generalizable to higher-income countries as they were predominantly carried out in lower-income countries (such as Kenya, Guatemala, Chile and Peru).
- There is always some uncertainty as to the true effectiveness of FABMs in the postpartum because breastfeeding itself tends to reduce fertility due to the suppressant action of prolactin on the HPO axis.
My thoughts after reading this systematic review:
While I would love to see more high-quality studies into the effectiveness of FABMs for the postpartum, I suspect that one of the main contributing factors to the dearth of research to begin with may be funding issues. Research studies are often funded by companies who stand to benefit from data about specific products/services that they own or provide – this is important because studies are expensive, and companies hope to be able to recoup some of the costs involved in investigating the effectiveness of their products. Not many companies stand to benefit from more studies into FABMs, except for small-scale FABM instructors and FABM training organisations, who usually cannot afford to fund studies to begin with. This is especially apparent when compared to the pharmaceutical companies behind other contraceptive methods such as IUDs, insertables and hormonal pills.
This particular systematic review appears to have been funded in part by KNDR Healthcare. KNDR Healthcare is the company behind the Reply OBGYN reproductive health clinic in the United States. Reply OBGYN also provide FABM training in a range of methods including Marquette Method, the Billings Ovulation Method, Sensiplan (a well-known Symptothermal Method), and Listen Fertility which is their own in-house FABM method relying primarily on mucus observations, with optional temperature and OPK monitoring. It’s great to see this healthcare company investing back into FABM research. I would love to see more reproductive healthcare providers here in Australia also offering in-house FABM instruction as this might also increase the likelihood of funding for further studies on the effectiveness of FABMs.

At the end of the day, opting to rely on a FABM for pregnancy prevention during the postpartum is a decision that only you can make. This decision should take into account a range of factors such as your reproductive intentions (how seriously you are needing to prevent a pregnancy), whether you have the time and financial resources (some methods such as the Marquette Method are more expensive than others), whether you are comfortable relying on cervical mucus observations alone, whether you are in a safe relationship with a partner who shares your reproductive intentions, and whether you are comfortable relying on a FABM during the postpartum given the lack of quality evidence of effectiveness rates.
Perhaps one of my biggest takeaways is that the postpartum is simply a notoriously difficult time to chart our fertility biomarkers for pregnancy prevention – and we can see this reflected in these relatively low typical-use effectiveness estimates. I hope that in future we have more innovation in this area so that postpartum individuals have safe and effective biomarker-based contraception available to them without such big question marks over effectiveness estimates.
This systematic review definitely gives me some pause as to whether it is advisable to rely solely on a FABM for pregnancy prevention during the postpartum for those who are low on the reproductive intentions scale (i.e. they have a serious need to prevent pregnancy). Personally, I think that if I were to be postpartum again in future, I would most likely combine coitus-dependent contraceptives with the Marquette Method. I would also layer this with the added cross-check of basal body temperatures using the Tempdrop smart thermometer to circumnavigate the difficulties of getting an accurate BBT due to nighttime parenting. You can read more about the Tempdrop here. And yes – I would definitely seek out Marquette Method instruction *before* birth (because time is decidedly short for learning new things during the immediate postpartum – I have learned my lesson here! 😅).
Do you have any thoughts on this systematic review? I would love to hear them – let me know in the comments below how you feel about this new information.

This article is brought to you by Jessie Brebner, a Symptothermal Method Instructor from the Gold Coast of Australia. Jessie is a passionate advocate for Fertility Awareness as a gateway to improved health, body literacy and reproductive empowerment. Jessie teaches the Symptothermal Method to people who are trying to conceive, and to people who are seeking a highly effective form of natural contraception.
1. Australian Bureau of Statistics, (1981–2016), Census of Population and Housing