As a Symptothermal Method Instructor, I am often floating in many corners of the internet at once! I am privy to conversations from a large swathe of different demographics across platforms such as Facebook, Instagram and Twitter. I love hearing from such a wide range of Fertility Awareness-Based Method (FABM) users who often reach out to chat via my DMs.
Without fail, one of the most common laments I hear is “I wish I had known about this at a much younger age – I can’t believe I only learned how my body worked in my 20s/30s/40s”. Oftentimes, the natural next iteration of this thought process is “I can’t wait to teach my daughter/teen/menstruating child about this information because I want them to have the empowerment and body literacy that I missed out on at their age”.
My response is sometimes a little tempered, for many reasons. I’ve decided to dive into some of the nuances involved in teaching teenagers about FABMs in this article. I hope that the points I cover will give parents and guardians pause for thought, and provide a basic framework of considerations that may help to provide safer experiences for teens who begin charting with a FABM.
Teenagers and menstruation in Australia
Here in Australia, a lack of education for teenagers on the menstrual cycle continues to result in menstrual taboos that have far-reaching consequences for girls and young women.
According to research by Plan International Australia, many boys and young men associated menstruation with words such as “messy”, “embarrassing”, “dirty”, and even “impure”.
Earlier research also found that almost a third of girls aged 10-14 were missing school and therefore falling behind in education due to embarrassment of being on their period and a fear of being teased.
In 2019, Libra was the first Australian menstrual product company to ever show a realistic depiction of period blood in a televised advertisement (#bloodnormal) – this was met with considerable controversy at the time due to the taboo that surrounds this normal bodily function.
This taboo can further be seen in research that shows that almost 70% of Australian girls would rather fail a subject at school than have their peers know that they are menstruating.
This data is devastating. Ongoing taboos are robbing girls and menstruators of their confidence, their dignity, and their education. Not only this, these taboos muddy their ability to feel carefree and spontaneous in their existence – how can we feel carefree when are living in fear of bullying regarding a natural, normal bodily function?
The state of menstrual taboos in Australia should not only concern us, but it should break our hearts. Women, girls and menstruators deserve better than this.
So, what’s the answer?
Education would be a great place to start.
How so? The same research mentioned earlier by Plan International Australia showed that 70% of boys who described their school education on periods as “good” also said that they felt comfortable discussing periods, indicating that education is key to breaking down these taboos.

Please note that this page contains affiliate links, meaning, at no additional cost to you, I may make a commission if you click through and make a purchase. This commission helps to keep this website up and running so that I can continue to provide resources for women to learn about Fertility Awareness. You can read more about this in the Advertising and Affiliates policy here.
Considerations of teenage FABM charting
Like most things in life, FABMs for teenagers is a complex, multifaceted topic with nuanced pros and cons that differ for each individual user.
That said, there are some considerations which spring immediately to mind, that I think parents and guardians should be aware of before considering a FABM for pregnancy prevention for their teen:
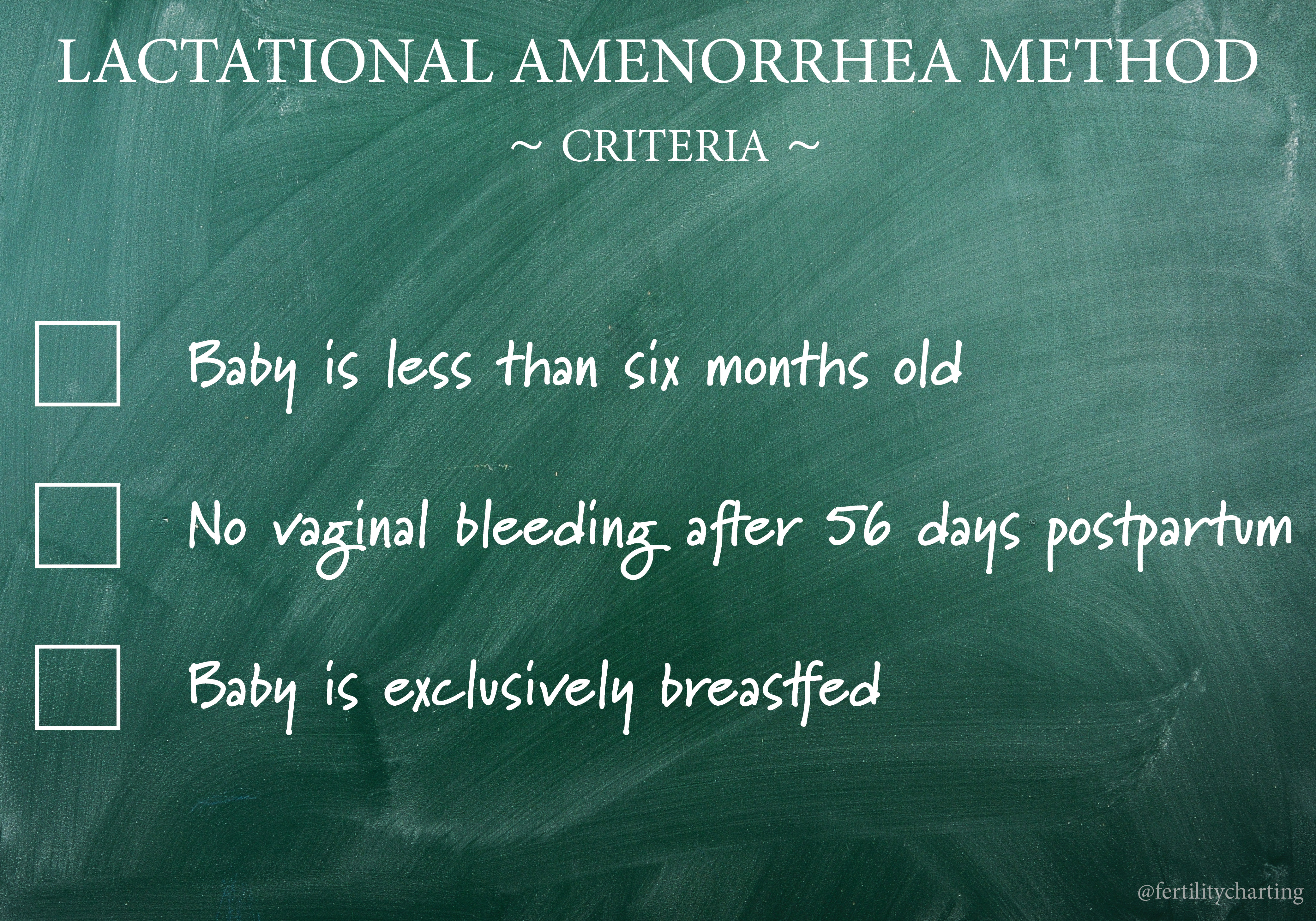
1.) Lack of evidence: Most FABM effectiveness rates are based on studies done of people in regular times of fertility. This means there is less evidence as to the safety and effectiveness of FABMs for pregnancy prevention during phases such as the teen years, postpartum, post-hormonal contraception and perimenopause. In my opinion, this is truly the largest drawback of recommending FABMs for teenagers – we simply don’t have enough evidence as to the safety of doing so.
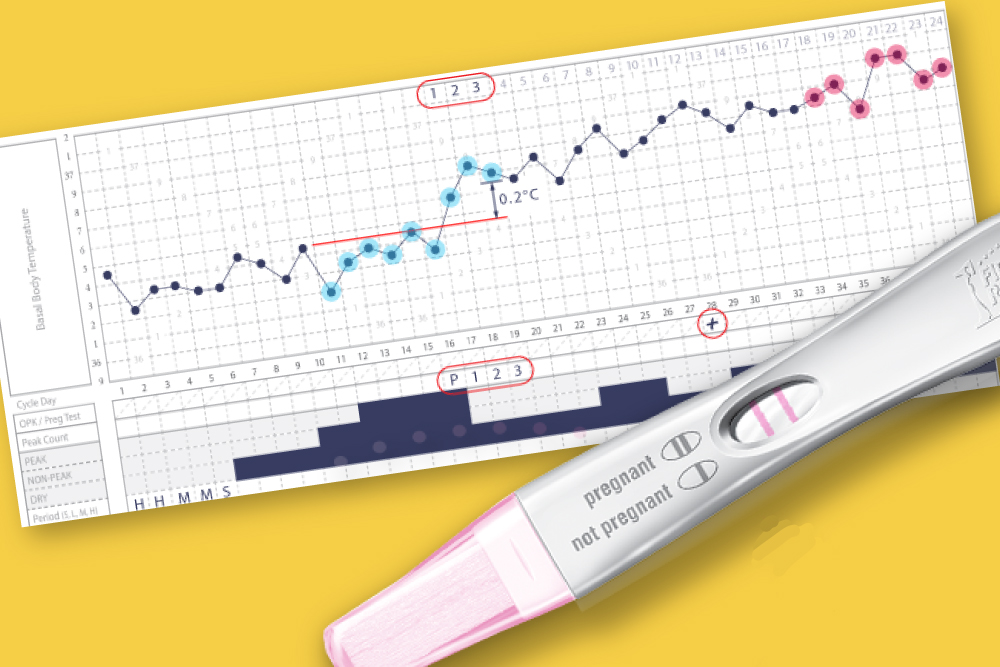
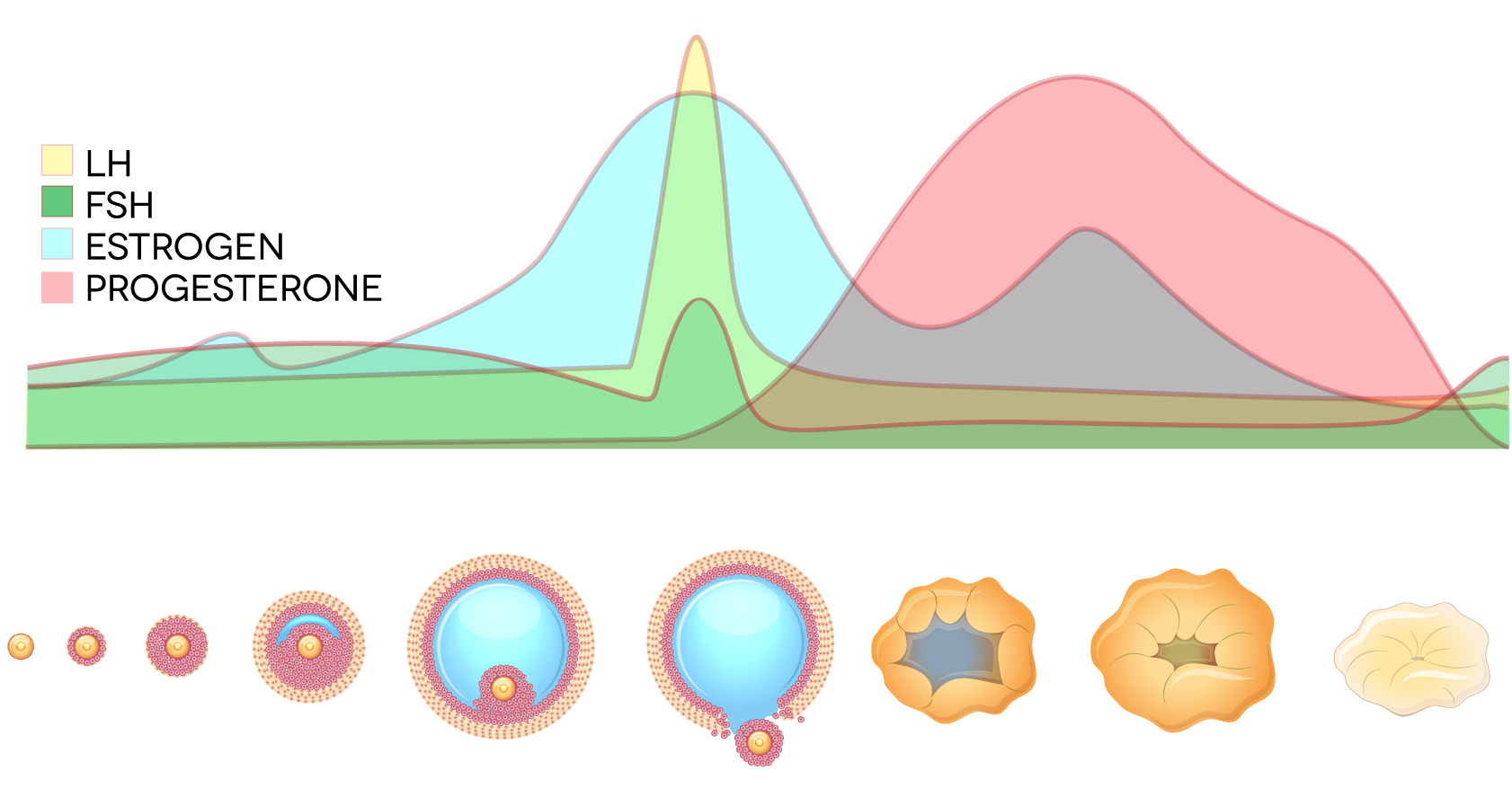
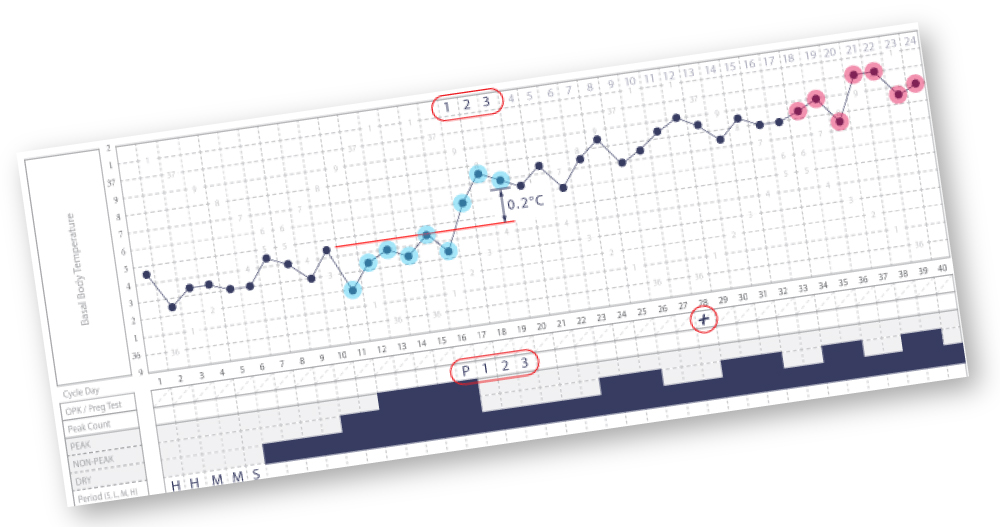
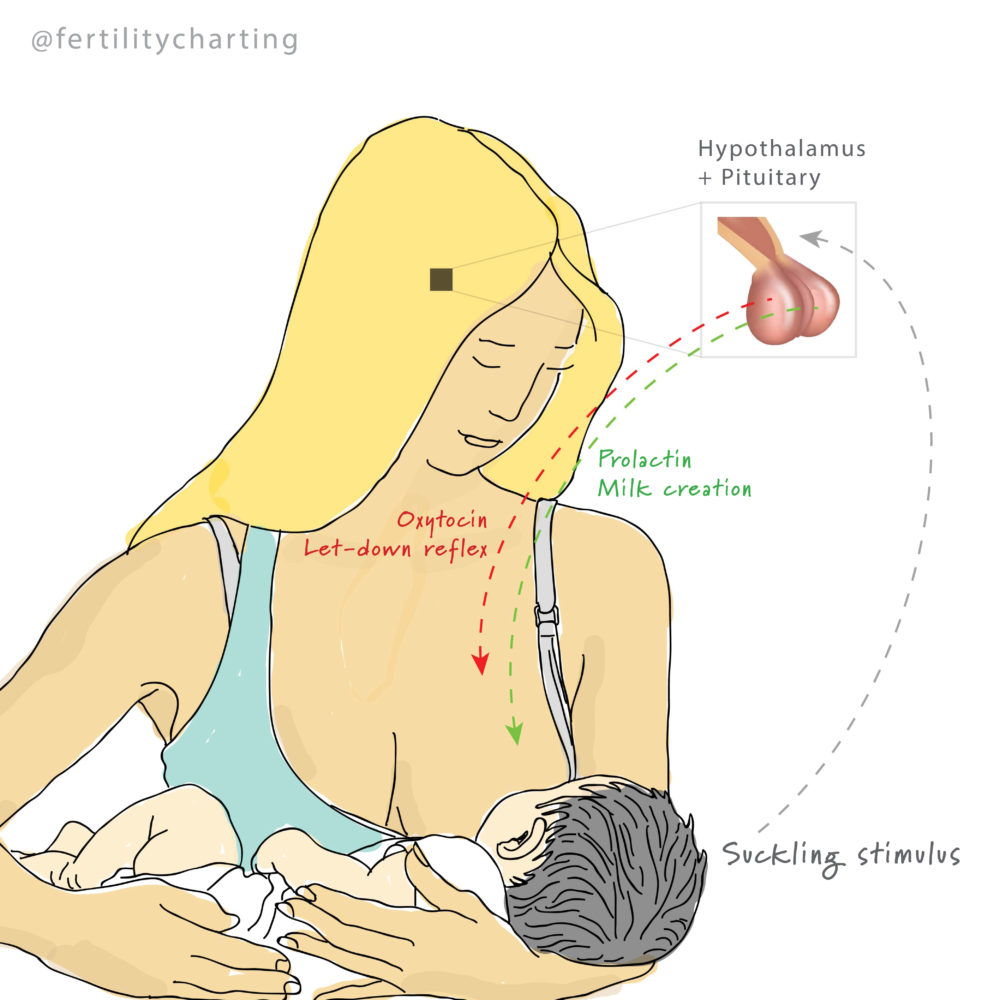
2.) Irregular cycles: Puberty can be considered a continuum of time during which the brain-ovary connection establishes and then stabilises. This connection is known as the hypothalamic-pituitary-ovarian (HPO) axis. Most teenagers will find that it takes time for ovulation to begin occurring regularly – and until it does, irregular cycles are common. This can be due to a mix of inputs including breakthrough bleeds, oestrogen-withdrawal bleeds, delayed ovulations, and short luteal phases. In essence, it takes time for the menstrual cycle to stabilise after puberty, and practicing a FABM during this time can be more difficult than usual.
3.) The prefrontal cortex: FABMs require a high level of user-involvement. Unlike “set it and forget it” contraceptives, using a FABM requires accurate daily observation of fertility biomarkers, accurate daily charting of findings into a paper chart or app, and modification of our sexual behaviour to prevent pregnancy during the method-identified fertile window. A high level of user-involvement may be less compatible with teenagers due to their underdeveloped prefrontal cortex. The prefrontal cortex is involved in rationality and impulse control and does not fully mature until around the age of 25. This may place teenagers at a higher risk of unintended pregnancy when relying on a contraceptive method that requires a high level of user-involvement.
4.) No protection against STIs: Unlike condoms, FABMs do not offer any protection against sexually transmitted infections (STIs). While abstinence is preferable from an STI protection perspective, sexually active teenagers should be educated on how to use condoms, and that they should be used during every sexual encounter. If your teen is sexually active and relying on a FABM for pregnancy prevention, condoms should still be utilised even if they are in a less-fertile or infertile phase of their menstrual cycle.
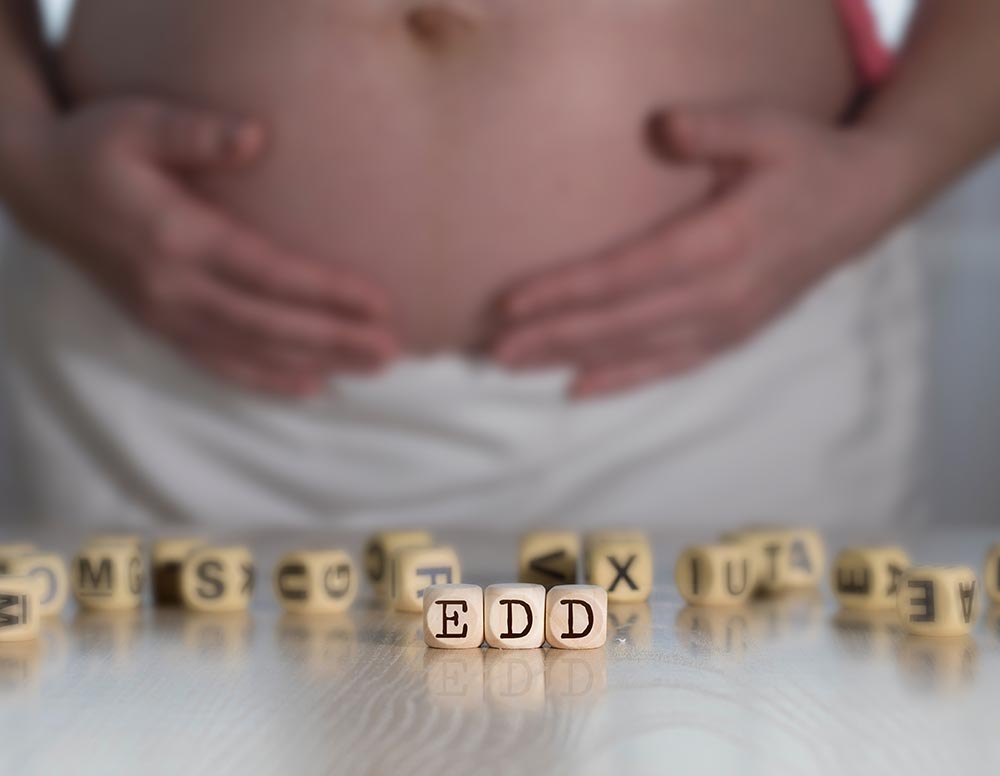
5.) Higher stakes: While an unintended pregnancy can be devastating at any age, the stakes are arguably higher for teenagers. Unintended pregnancy can have far reaching adverse social and economic outcomes which may negatively impact the life trajectory of teenagers. In addition, adolescent pregnancies can pose more health risks for the mother and infant than an adult pregnancy would.
Benefits of FABMs for teenagers
While the above considerations should be taken very seriously, there are also numerous and significant benefits to learning about how our bodies work as teenagers! Fertility Awareness-Based Methods (FABMs) bring empowerment, body literacy and insight into our own inner workings. They can provide the map that allows us to easier navigate our changing emotions and mental/physical capabilities across the different phases of the menstrual cycle. This information can be life-changing, and teenagers should have access to begin their learning process here.
With all that said, here are my recommendations if you have a teenager who is interested in learning how to chart with a FABM, or if you have a teenager who you feel would benefit from increased cycle and body literacy:
1.) Focus on charting for body literacy: Instead of focusing on using a FABM for pregnancy prevention, use this knowledge instead as a springboard toward body literacy. Many teenagers are lacking the most fundamental basics when it comes to understanding their reproductive anatomy and how their menstrual cycle works – this is where FABM education really shines.With basic education on anatomy, the menstrual cycle, cervical mucus and basal body temperature, teenagers can:
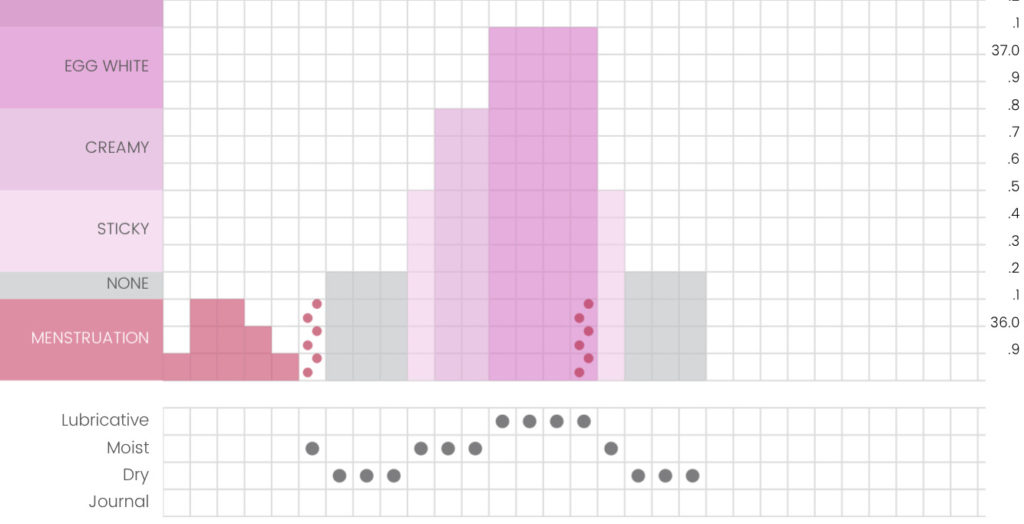
- Demystify cervical mucus
- Confirm whether ovulation is occurring
- Accurately predict the onset of their periods
Demystifying cervical mucus alone is hugely valuable given so many teenagers worry that something is wrong with them when they first begin to experience cervical mucus during puberty. Predicting the next menstrual bleed by watching for a luteal-phase temperature drop or counting days of the luteal phase empowers teenagers to prepare in advance for a bleed and allays some of the anxiety that surrounds an unexpected bleed (although breakthrough/withdrawal bleeding can still be common during puberty).
2.) Shine the spotlight on their cyclical nature: Puberty can be a disconcerting time of great change for teenagers who may begin dealing with uncomfortable physical and mental symptoms as their bodies change. It can be empowering for teenagers to understand that their moods and emotions and physical capabilities can be impacted by their menstrual cycle. For example, by tracking diligently they may notice that they are more likely to experience cravings, fatigue and irritability or sadness in the lead-up to their period. This knowledge can act as a roadmap for teens to navigate their cyclical nature. It also provides reassurance that these experiences can be very normal, especially while their cycles are regulating and ovulation gradually becomes more robust with greater levels of progesterone produced.
3.) Chart to monitor reproductive health: Charting can be a great tool for teens to stay on top of health issues during puberty. If issues such as heavy bleeding, amenorrhea, vaginal infections, consistently delayed ovulations and/or irregular cycles are present, using a FABM can encourage us to seek medical diagnoses and assistance. It’s better to be informed than not, and FABMs are a great way to keep on top of our reproductive health.
4.) Allow the HPO axis time to mature: It takes some time for the HPO axis to mature during puberty. During this time, it’s normal for teens to experience irregular cycles. Author Sarah E. Hill states that we have a blind spot when it comes to how the Pill impacts our brains by switching off our sex hormones. Is it possible that we benefit our teenage brain development by allowing our HPO axis to mature instead of shutting it down completely with the Pill? A fascinating topic to dive into and I recommend reading Hill’s book ‘This is Your Brain on Birth Control’ if you’re curious about this subject.

Where to from here?
If you would like your teenager to learn a Fertility Awareness-Based Method (FABM), there are a few things I recommend:
1.) Start out slow: Focus entirely on charting for body literacy to begin with. Begin by simply tracking menstruation dates, and then slowly layer in things like cervical mucus and sensation charting, secondary fertility signs (such as acne and bloating), and finally adding in basal body temperatures. Focus on how to use these biomarkers to predict when their next period will arrive, and how to understand themselves better as cyclical beings. Pregnancy prevention should not even be a part of the story, at least at the beginning. As your teenager grows and matures, you may want to introduce the concept of using a FABM for pregnancy prevention, but at least initially, the focus should simply be on body literacy.
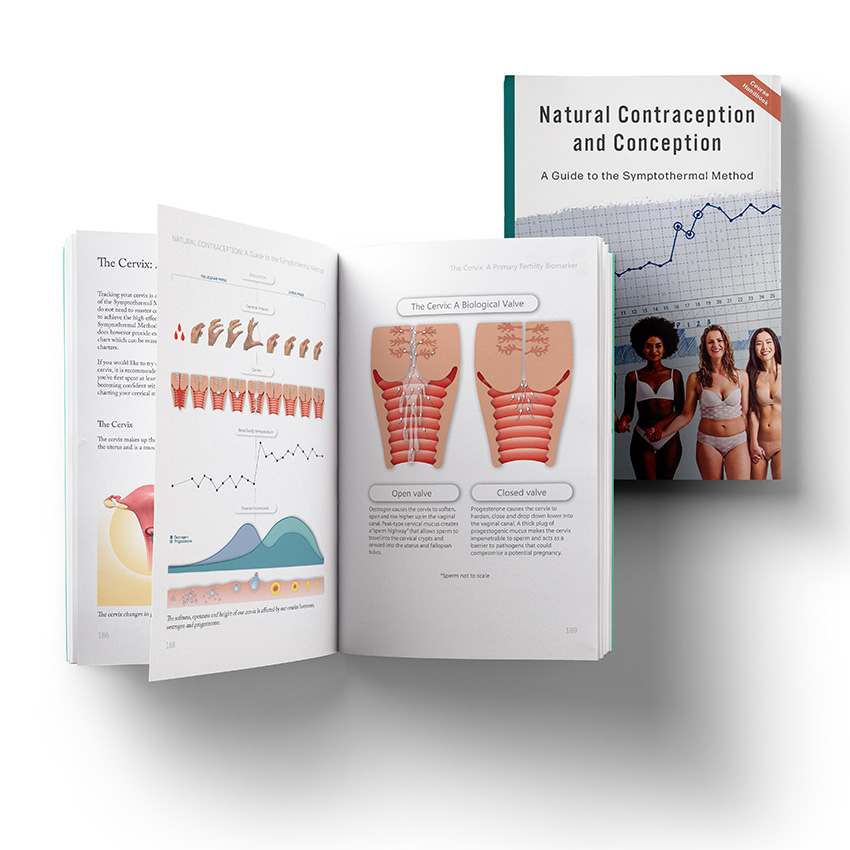
2.) Hire a qualified instructor: If you do feel like your teenager is interested in learning how to rely on a FABM for pregnancy prevention, hire a qualified instructor of a specific method. Now is not the time to cobble together a rough method based on your own knowledge. Now is not the time to piece together snippets from podcasts, books, and social media. Maybe you are already an accomplished and competent FABM charter yourself, but maybe you’re not – and the only way to find out for sure is either an accidental pregnancy or taking a FABM course to double-check your knowledge – I know which one I prefer! Personally, I think SymptoPro has one of the most comprehensive Symptothermal educator-training programs and I would feel safer referring teens to a SymptoPro instructor over some other method instructors. You can find SymptoPro instructors here: https://symptopro.org/services/learn.html
3.) Start early: Invest in some relevant books for your teenager to read and learn from at a younger age. Two great options are:
4.) Look into teen-specific FABM education: You may be comfortable taking a teen-specific FABM course with your child.
*Some of these courses may provide general body literacy education, and not necessarily actual charting instruction.
*Some of these courses are provided by Catholic organisations. This means they are likely to focus on abstinence and general body literacy (as opposed to using a FABM for pregnancy prevention).
TeenFEMM classes: FEMM is a secular organisation; however, they are funded by and have links to anti-abortion groups/individuals, which some charters may be uncomfortable with. You can read more here if this is a concern: https://www.theguardian.com/society/2019/jul/29/us-federal-grants-femm-app-natural-birth-control
Mother-Daughter courses run by Fertility Science Institute (FSI): FSI was launched by FABM organisation Couple to Couple League (CCL). There are three courses to choose from depending on the age of your teen. CCL and FSI are Catholic pro-life organisations and are morally opposed to abortion, hormonal birth control, barrier methods such as condoms, and artificial reproduction technology such as IVF/IUI.
Cycle Show course by the Guiding Star Project: Guiding Star Project are a Catholic pro-life organisation and are morally opposed to abortion, hormonal birth control, barrier methods such as condoms, and artificial reproduction technology such as IVF/IUI. The Cycle Show is based on the teachings of the book ‘What’s Going on in My Body?’ by Elisabeth Raith-Paula.
Period Ready Parent-Teen eCourse by Bright Girl Health: A secular offering by Bright Girl Health Australia. Perfect for teens/tweens approaching their first period or navigating the first few years of menstruation. Designed to equip parents to support teens with body positivity and period pride. Includes comprehensive eBook, activity worksheets and video modules.
Body Talk Basics “Conversations About Puberty for Moms and Daughters”: A secular offering by Megan of Body Talk Basics. A gentle overview and introduction to an empowered puberty. Includes 3 hours of video modules, a workbook and a physical handbook.

This article is brought to you by Jessie Brebner, a Symptothermal Method Instructor from the Gold Coast of Australia. Jessie is a passionate advocate for Fertility Awareness as a gateway to improved health, body literacy and reproductive empowerment. Jessie teaches the Symptothermal Method to people who are trying to conceive, and to people who are seeking a highly effective form of natural contraception.



















 – however this method must be undertaken with an instructor as it involves off-label use of the monitor via a complex re-setting pattern.
– however this method must be undertaken with an instructor as it involves off-label use of the monitor via a complex re-setting pattern.