What does this mean? There is little scientific evidence for the safety and effectiveness of any type of FABM for pregnancy prevention during the postpartum. In addition, the evidence we do have is considered to be of low quality.
You can read more about this latest 2022 systematic review here.
A special note:
I would like to preface this article with the caveat that postpartum charting can be very challenging as it is a time of hormonal change and uncertainty while fertility slowly returns after birth. This can result in long periods of abstinence or barrier use that can be frustrating for some users. In addition, once-reliable fertility signs such as cervical fluid and basal body temperature can become confusing to track and special postpartum rules must be applied. For this reason, I don’t recommend that you learn a Fertility Awareness-Based Method for the first time during the postpartum period unless you will be working very closely with an instructor. You can find an instructor by clicking here.

Birth is a radically transformative event. If you’ve recently expanded your family by birthing a child you’re likely very aware of this! You may be navigating new challenges and demands as you grow into this new facet of your identity.
These challenges can be both mental and physical. Even if you’ve been cleared to resume intercourse by your healthcare provider you may be reluctant to “get back on the horse” as the saying goes. Every woman’s experience will be different but common causes of low libido centre around:
- perineal healing,
- c-section scar healing,
- sleep deprivation,
- body image issues,
- mental health issues (such as PPD and/or PPA),
- emotional overexertion (or a feeling of being “touched out”), and
- vaginal dryness as a result of low oestrogen due to breastfeeding.
Or, perhaps you’re on the other side of the equation and have been back in the sheets since week three!
Either way, it’s best to tackle the issue of contraception early on so that when the time comes you and your partner have a game plan ready.
During pregnancy, ovulation is suppressed due to high levels of placental progesterone and oestrogen. High levels of these hormones have a suppressive effect on the release of luteinising hormone from the pituitary gland in your brain. Luteinising hormone is required for the maturation and release of an ovum (egg) from your ovaries; therefore, suppressed luteinising hormone = no ovulation.
How soon you begin ovulating after giving birth will depend on whether or not you choose to breastfeed, and for how long. Why is this? Because breastfeeding suppresses ovulation – in some situations. Read on for more information.
Please note that this page contains affiliate links, meaning, at no additional cost to you, I may make a commission if you click through and make a purchase. This commission helps to keep this website up and running so that I can continue to provide resources for women to learn about Fertility Awareness. You can read more about this in the Advertising and Affiliates policy here.

“I will not be breastfeeding”
As the saying goes – fed is best! Many mothers will end up using formula due to work schedules, health conditions, difficulties with breastfeeding and pumping, societal norms, lack of support or simply due to personal preference. If you choose not to breastfeed (or are unable to), you should be aware that your fertility will return much more rapidly than those who are breastfeeding. This also applies if you are unable to exclusively breastfeed (continue reading below for a definition of exclusive breastfeeding). If you are not breastfeeding, or only partially breastfeeding and you wish to use a Fertility Awareness-Based Method (FABM) you will need to start charting your fertility biomarkers within two-three weeks of giving birth. This is because it is possible to ovulate as early as the fourth week postpartum if you are not breastfeeding! On average though, (if bottlefeeding) your first menstrual bleed is likely to return around eight weeks postpartum, with ovulation first occurring for 94% of women in their second menstrual cycle following birth. [1]

“I will be breastfeeding”
Many mothers will choose to breastfeed, especially with the World Health Organisation (WHO) recommending that infants be exclusively breastfed up until the age of six months. The WHO also recommends continued breastfeeding (in addition to supplemental foods) up until the age of two years. In Australia, the Department of Health recommends exclusive breastfeeding up until six months, with supplemental feeding continuing up until 12 months (and beyond if the mother and infant wish to continue). If you’re choosing to breastfeed, it may help to understand exactly how and why breastfeeding will affect your fertilty.
Prolactin – The Breastfeeding Hormone
Prolactin is a hormone released by the pituitary gland in your brain. It causes your breasts to secrete milk. During pregnancy, prolactin levels steadily increase, but lactation is suppressed due to high levels of placental oestrogen. During the 48 hours after birth, oestrogen levels drop rapidly and lactation can finally begin in earnest. These high prolactin levels after birth will not be maintained or increased unless suckling occurs.
Suckling of a baby on the breast stimulates nerves within the areola. These nerves then send a message to the hypothalamus and pituitary glands to produce a surge of prolactin and oxytocin. The surge of prolactin creates more milk, while the surge of oxytocin stimulates the “let-down reflex” that brings milk to the nipple.
The surge of prolactin begins to dissipate within three hours unless the breasts are stimulated during this time with further suckling.
To establish a successful breastfeeding relationship with the baby, it is recommended that this suckling begins as soon as possible after birth – preferably within the first hour of life. The WHO have a number of other recommendations to promote successful breastfeeding such as immediate and uninterrupted skin-to-skin contact after birth. You can read these recommendations here and here.
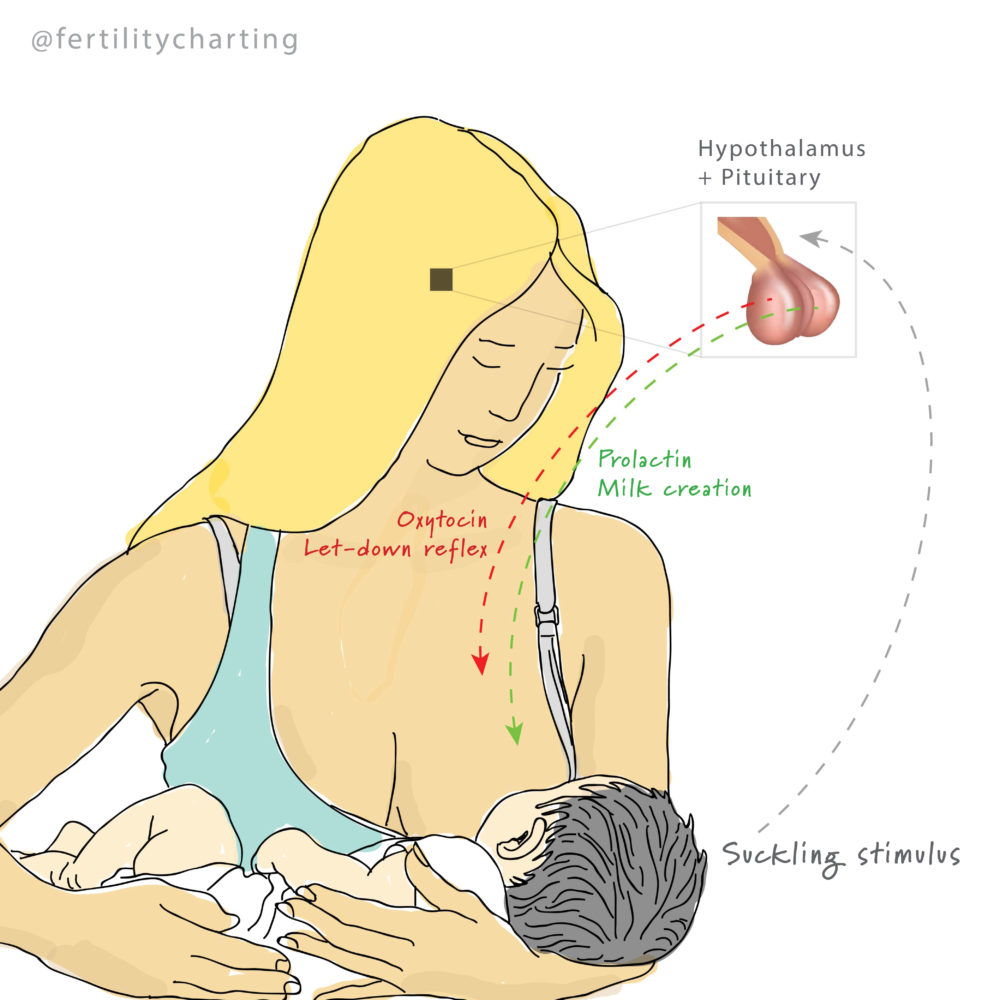
How Does Prolactin Affect My Fertility?
Prolactin has a suppressant effect on fertility because it disrupts the ability of the pituitary gland to release Follicle Stimulating Hormone (FSH) and Luteinising Hormone (LH). FSH stimulates the growth of follicles within your ovaries (follicles are small fluid-filled sacs that each house an ovum). Around the middle of your menstrual cycle, a surge of LH matures one ovum (or occasionally two or more in the case of twins and triplets). [You can read more about multiple ovulation here]. The surge of LH simultaneously causes the matured ovum to rupture through the follicle and ovarian wall, to be collected by the waiting fallopian tube. In this way, both FSH and LH are crucial for the event of ovulation to occur. If these hormones are suppressed (as is the case when prolactin levels are sustained at high enough levels), ovulation cannot take place.
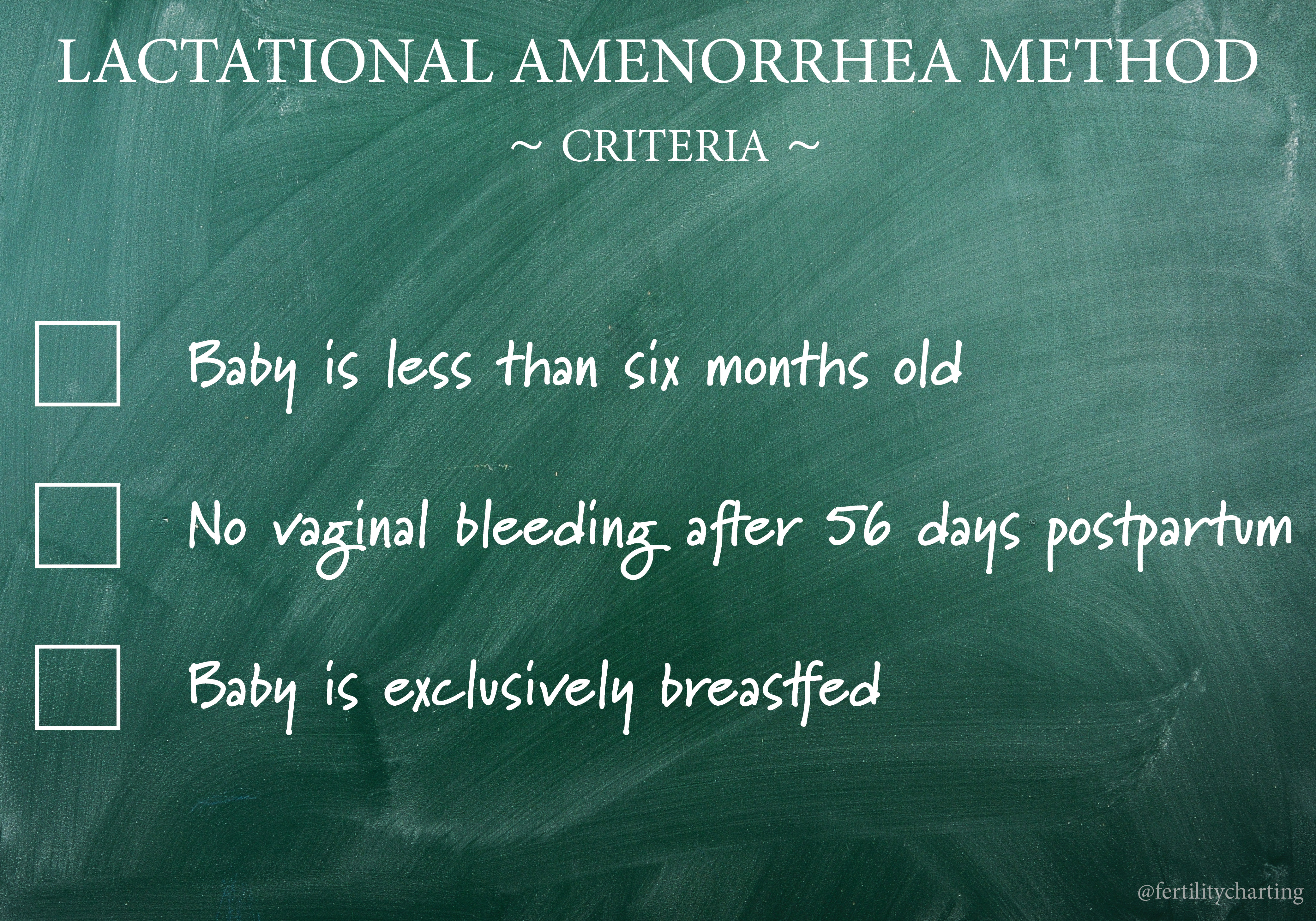
LACTATIONAL AMENORRHEA METHOD
Harnessing the contraceptive power of prolactin in the first six months after birth is known as the Lactational Amenorrhea Method (LAM). This natural method of contraception is proven over 98% effective [2] but it requires diligent adherence to three specific rules:
- Baby must be less than six months old, and
- Mother must not experience any vaginal bleeding after the first 56 days postpartum, and
- Mother must be exclusively or almost exclusively breastfeeding.
If any of the above three criteria are not met at any stage, prolactin levels can quickly drop and ovulation could occur. Due to our modern lifestyles it is very difficult to fully meet all of the LAM criteria, and because of this, I highly recommend working with an instructor to ensure that your breastfeeding relationship meets the criteria of LAM. You can find an instructor to work with by clicking here.
I also recommend that if you wish to rely on LAM as postpartum contraception but you absolutely do not want to fall pregnant, that you chart your fertility in tandem to practising LAM from as early as possible after birth. It’s also a good idea to incorporate a concept known as ecological breastfeeding. Both postpartum fertility charting and ecological breastfeeding are covered in more detail below.
Menstrual Bleeding After Day 56:
- This is defined as any bleeding after day 56 that lasts for two or more days and requires sanitary protection for at least one of those days. If this occurs, it means that fertility is returning and LAM no longer applies.
Exclusive Breastfeeding:
- Breast milk is the only sustenance the baby receives – he or she does not receive any other liquids or solids that are not breast milk. (If it is medically necessary to provide baby with other liquids or solids, the parents must understand that the contraceptive effect will lapse).
- The gap between breastfeeds should not exceed 4 hours during the day or 6 hours during the night. Reducing the frequency or duration of breastfeeds will reduce the effectiveness of LAM.
- No pacifiers or dummies are used. Babies suckle for comfort, not just food – comfort suckling plays an important role in the secretion of prolactin.
- Pumping breast milk (whether by hand or pump) has not been fully studied and will reduce the effectiveness of LAM.
The longer the duration of the breastfeed, the higher the level of prolactin that is released. Prolactin reaches higher levels during the nighttime hours – so once baby begins to sleep for longer periods at night, prolactin levels may drop low enough for fertility to return.

Unfortunately, the nature of LAM is such that it is not accessible to all women who would be interested in using it. In today’s society, many women have responsibilities and schedules that make it impossible to exclusively breastfeed for the first six months of infant life. In Australia, 11% of mothers have already returned to work at three months postpartum [3], and only 15% of babies are still being exclusively breastfed at the age of five months [4]. In the United States where there is no universal paid parental leave system, a whopping 58.6% of women have returned to work within three months of giving birth [5].
If you choose to partial breastfeed but cannot commit to exclusive breastfeeding, you will need to start charting your fertility biomarkers within two-three weeks of giving birth. Return of fertility may be quick or it may be delayed many months – during this time special postpartum charting rules will apply. It is highly advisable to work with an instructor during this time and you can find an instructor by clicking here.
Even for those women who could theoretically meet the requirements of LAM, the below meme might explain why not all choose to pursue this option!
What Happens When LAM No Longer Applies To Me?
At some point, you will no longer meet all three criteria to continue using the Lactational Amenorrhea Method. Perhaps your period returns before you reach the six month mark, or work commitments mean you can no longer exclusively breastfeed, or your baby begins to sleep through the night. Or perhaps your baby simply reaches six months of age and LAM no longer applies.
When LAM no longer provides natural infertility, most women are still in need of some form of contraception. The WHO recommends that couples wait a minimum of two years before trying for another baby [6]. This can be important to reduce the risk of adverse maternal, perinatal, neonatal and infant health outcomes.
How you choose to manage your fertility during this time will depend on how seriously you are wanting to avoid a pregnancy. Many women will already be planning their next pregnancy and will not be overly concerned on the spacing between births. Others will be at a life-stage where they are finished planning their family and don’t wish to fall pregnant ever again (and are perhaps looking into vasectomy or tubal ligation options).
Depending on your reproductive intentions, there are two natural methods available to you – FABM charting and ecological breastfeeding.
FABM CHARTING FOR THE POSTPARTUM

If you’re covered by the Lactational Amenorrhea Method and are seriously wanting to avoid a pregnancy, it’s important that you begin charting your fertility signs at the fifth month postpartum (at least two weeks before you reach six months postpartum).
This is because ovulation can occur either before or after your first menstruation/bleed; in fact, approximately 60% of breastfeeding parents who are past six months postpartum will ovulate before they have their first period. If you are part of this 60% you will want to be tracking your fertility signs to avoid falling pregnant on your first postpartum ovulation! In some cases though, it can take around three cycles for fertility to fully return – the first cycle is sometimes anovulatory, followed by a cycle or two with a short luteal phase not supportive of implantation.
How soon your fertility returns will depend on how your breastfeeding relationship plays out. Remember, frequent suckling stimulates the release of prolactin which has a suppressant effect on ovulation. For those who abruptly wean with the introduction of solids after the six month mark, fertility can quickly return. For those who wean very gradually this process can sometimes take longer.

This can be a confusing time for those who are using a FABM to chart – I liken the postpartum time to a kind of fertility “no-mans land“. This is because you no longer have the protection of the Lactational Amenorrhea Method, but you also don’t have regular, ovulatory cycles. It can mean long periods of abstinence or barrier-use (such as condoms) as you wait to try and catch your first ovulation.
In addition to this, postpartum charting presents two other unique challenges:
- Cervical mucus can present differently due to breastfeeding
- Waking frequently through the night with your baby can make it difficult to obtain an accurate basal body temperature reading
While you’re in this “no-mans land” or “cycle zero” as most refer to it, it is very important that you work closely with an instructor who is experienced in postpartum charting. You’ll need to be very confident at tracking a fertility sign that is influenced by oestrogen so that you can catch your first ovulation. This is because your temperature is only going to rise after ovulation has already occurred, which doesn’t offer you any protection against pregnancy considering sperm can survive up to 5-7 days in the reproductive tract. Once your temperature has risen it is too late to take back that unprotected sex from four nights ago!
If you’re only tracking BBT, you’ll need to be investing in a time machine!
Fertility signs that are influenced by oestrogen are your cervical fluid and your cervical position. Because oestrogen levels rise in the lead-up to ovulation, it is important that you are very confident in charting these signs.
Symptothermal Method or Billings Ovulation Method charting for the postpartum
If you’re using a Symptothermal Method, there are special FABM rules that must be used for the postpartum. Special rules are required because cervical mucus is often affected by breastfeeding. These rules help each individual person to identify their personal “Basic Infertile Pattern”. It is for this reason that I don’t recommend you attempt to self-teach a FABM during the postpartum. Instead, I recommend working closely with an instructor who can carefully guide you to learn postpartum charting rules. You can find an instructor by clicking here.
The Symptothermal Method relies on both cervical mucus and basal body temperature (BBT). BBT only rises in a sustained fashion after ovulation has already occurred. Because ovulation can be significantly delayed in the postpartum, this means that BBT is not a very useful fertility biomarker for this specific life stage. Instead, you are relying on fertility biomarkers that are influenced by oestrogen, such as cervical mucus and changes in the cervix itself. It can be beneficial to pay closer attention than usual to cervix tracking – in many cases where cervical mucus remains confusing, the cervix provides the first clue that fertility is returning. Again, I recommend working with an instructor to learn about cervix tracking as the position of your uterus can sometimes affect how your cervix will be positioned during the fertile window.
One of the strengths of the Symptothermal Method is that we are always cross-checking two separate biomarkers (mucus and BBT) against one another. This means that Symptothermal mucus-checking protocols are often relatively “basic” because they always have the added security of a BBT cross-check. However, this can be a weakness of relying solely on Symptothermal Method postpartum protocols that are often of quite a basic nature in regards to cervical mucus.
In fact, if ovulation is delayed due to breastfeeding, I recommend that you seek out a cervical mucus only method such as the Billings Ovulation Method. Cervical mucus-only FABMs have highly detailed mucus-only protocols that are more well-suited to the postpartum than Symptothermal protocols. You can find Billings Ovulation Method instructors in the Instructor directory.
Marquette Method Charting
If you feel as though charting with the Symptothermal Method or the Billings Ovulation Method during the postpartum will simply be too difficult for you, it may pay to look into the Marquette Method. The Marquette Method is fantastic for postpartum charting because it simply involves testing your urinary hormone metabolites each morning using a special fertility monitor that measures oestrogen and luteinising hormone. You can find a Marquette Method instructor by clicking here. The Marquette Method also has a dedicated and active facebook group that you can join for more information – click here to take a look. If you’re interested in using the Marquette Method, keep in mind that it is a Catholic organisation and religious content will likely feature in the learning materials. The Marquette Method has a very high effectiveness rating (on par with the Symptothermal Method) and the fact that it involves very objective digital urine testing can be a reassurance for users who definitely want to avoid a pregnancy.

 – however this method must be undertaken with an instructor as it involves off-label use of the monitor via a complex re-setting pattern.
– however this method must be undertaken with an instructor as it involves off-label use of the monitor via a complex re-setting pattern.Barrier Methods
Finally, if you have a strong preference for a natural method of contraception, but are struggling to maintain a FABM charting practise while coping with the demands of caring for a new baby, don’t forget that barrier methods are also an option. Condoms are generally the most popular and easily accessible. If you used a diaphragm prior to birth, don’t forget that you will likely need a re-fitting to a larger size after birth.
ECOLOGICAL BREASTFEEDING
For those who are less concerned about falling pregnant and simply wish to naturally space their next child, a practise known as ecological breastfeeding may be a suitable option. Ecological breastfeeding is a term coined by John and Sheila Kippley of the Catholic organisation Natural Family Planning International. It involves exclusive breastfeeding (as outlined for LAM), but also includes six other standards that must be met. These standards can also be used to bolster the effectiveness of LAM.

The protocol encourages a very natural type of mothering and is said to extend amenorrhea (absence of periods) out until 14.5 months on average. Keep in mind that this is just an average – your period could return much earlier than this. For this reason, the method is not suitable for those who absolutely want to avoid an unplanned pregnancy.
The Seven Standards:
- Breastfeed exclusively for the first six months of life
- Pacify or comfort the baby at your breasts
- No bottles or pacifiers
- Sleep with your baby for night feedings
- Sleep with your baby for a daily-nap feeding
- Nurse frequently day and night and avoid schedules
- Avoid any practice that restricts nursing or separates you from your baby
As you can see, it can be extremely difficult for a mother to meet these guidelines if she has responsibilities (such as a career or other small children) that will separate her from her baby. I don’t know very many mothers who have the option to nap with their baby every day!

In addition, almost all major health organisations (including Health Direct Australia and American Academy of Pediatrics) recommend against co-sleeping to reduce the risk of Sudden Infant Death Syndrome (SIDS). Interestingly, breastfeeding has been shown to reduce the risk of SIDS. The majority of SIDS cases also involve hazardous risk factors that are largely preventable. If you choose to co-sleep, the Australian Breastfeeding Association have a fact sheet of guidelines which you can access by clicking here. Unicef also have a guide for health professionals to discuss co-sleeping with their patients and you can read that guide here.
To read more about ecological breastfeeding you can click here for a pdf, or click here to purchase the book The Seven Standards of Ecological Breastfeeding: The Frequency Factor by Sheila Kippley.
However you choose to navigate the postpartum, rest assured you have a number of effective natural methods that you can turn to for contraception. A qualified Fertility Awareness Educator will be able to guide you toward the method that will be most suited to your individual situation. You can find a Fertility Awareness Educator by clicking here.
This online resource is not a substitute for qualified medical advice. Please ensure you discuss your postpartum contraceptive plan with a health professional and/or Fertility Awareness Educator to ensure you are receiving accurate guidance.
This article has been referenced from a number of sources including NFPTA-UK teaching materials, The Complete Guide to Fertility Awareness by Jane Knight, Taking Charge of Your Fertility
by Toni Weschler, and The Seven Standards of Ecological Breastfeeding: The Frequency Factor
by Sheila Kippley.
The below specific references have also been cited:
[1] Howie, P. W ., McNeilly, A. S., Houston, M. J., Cook, A., and Boyle, H. Fertility after childbirth: Post-partum ovulation and menstruation in bottle and breast feeding mothers. Clinical Endocrinology (Oxford), 17(4):323–332, Oct 1982.
[2] https://www.contraceptionjournal.org/article/S0010-7824(97)00040-1/fulltext
[3] https://aifs.gov.au/publications/timing-mothers-return-work-after-childbearing/results
[4] Australian Institute of Health and Welfare 2011, 2010 Australian National Infant Feeding Survey: Indicator Results. Canberra: AIHW. URL: http://www.aihw.gov.au/publication-detail/?id=10737420927
[5] https://www.census.gov/prod/2011pubs/p70-128.pdf
[6]https://apps.who.int/iris/bitstream/handle/10665/69855/WHO_RHR_07.1_eng.pdf;jsessionid=C5713FDEE2A70056E45196212478BB20?sequence=1



Wow Jess! I continue to be blown away by your depth of research and knowledge. This is an invaluable resource for women wanting to use FAM in the postpartum.
Thank you so much Nathalie! I really appreciate the positive feedback – a big thank you to you! Jess x
Wondeful and valuable information here. Just what I had been looking for with my husband.
I’m so glad to hear it! Thank you for the positive feedback. All the best as you plan for your postpartum!