What Is The Symptothermal Method?
Each menstrual cycle, your body ovulates approximately two weeks before your next period. The egg your ovaries release lives for around 24 hours. Sperm can survive up to 5-7 days in your reproductive tract. With the combined lifespan of sperm and egg, you have an approximate 6-9 day biological fertile window each menstrual cycle.
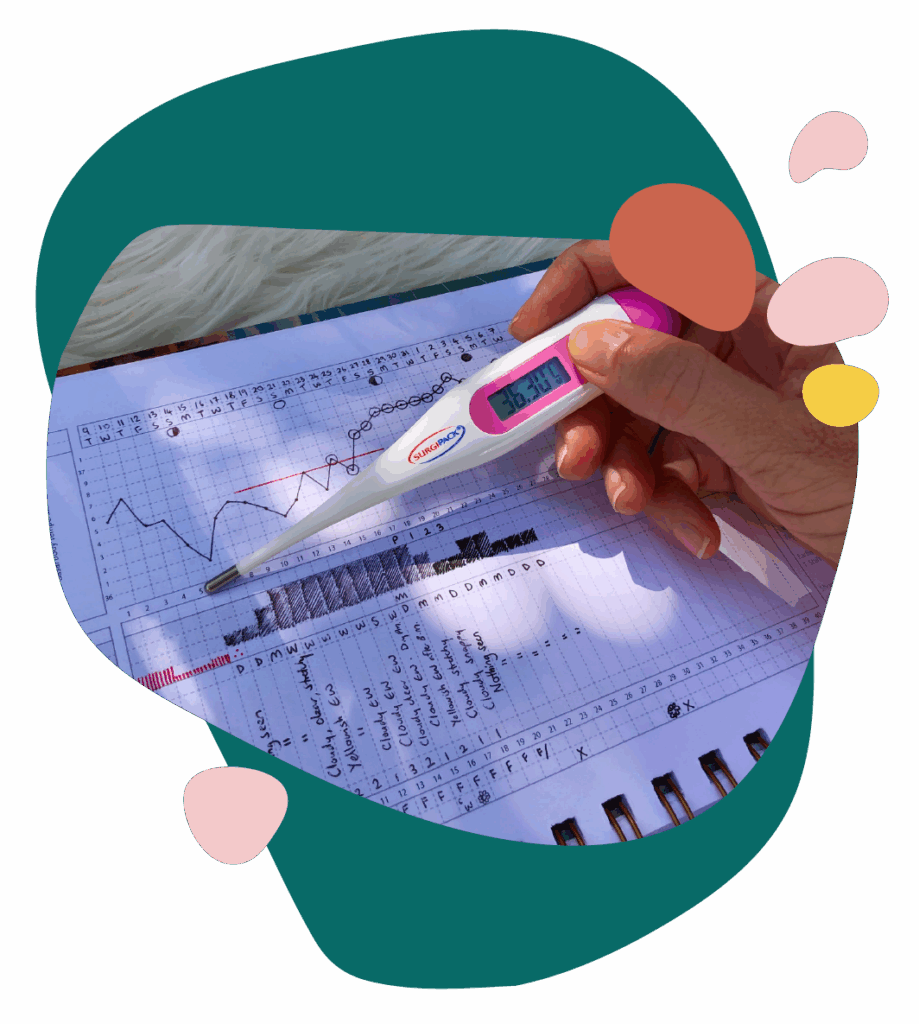
By carefully tracking your cervical mucus and your basal body temperature, you can know when you are approaching this fertile window, and when you have passed this fertile window.
The Symptothermal Method has very specific rules to follow to ensure accuracy. It’s never possible to pinpoint the exact day of ovulation in advance of it occurring. Because of this, the Symptothermal Method will always add a buffer of at least several days either side of your true biological fertile window. This is known as the “method-identified fertile window”.
What you choose to do with this information is a matter of personal choice. The Symptothermal Method can be used as a highly effective form of natural contraception, as a way to optimise your chances of falling pregnant each cycle, or as a window into your hormonal health. The Symptothermal Method is very versatile and can be used to achieve all of these reproductive goals at different points in your life.
How Does The Symptothermal Method Work?
Cervical mucus is influenced by oestrogen and progesterone and changes in consistency, colour and volume throughout your menstrual cycle. As oestrogen rises in the lead-up to ovulation, you’ll notice changes to the colour, amount, and texture of your cervical mucus. You’ll also notice the sensation at your vulva becomes increasingly wet and slippery. After ovulation, your cervical mucus dries up. Tracking changes in your cervical mucus gives you advance warning that ovulation may be approaching, and helps to confirm when ovulation may have passed.
After ovulation, your ovaries produce a hormone called progesterone. Progesterone causes your basal body temperature to heat up. By tracking this small rise in temperature with a special basal body temperature thermometer, you can identify when ovulation has passed.
Symptothermal Method users cross-check their cervical mucus observations against their temperature readings to know with high accuracy when ovulation has passed each menstrual cycle.
For many Symptothermal Method charters, there is also a time of infertility at the start of the menstrual cycle (during your period and just after it). This time is identified by tracking cervical mucus, and cross-checking mucus observations against calculation rules. Calculation rules use data from past menstrual cycle lengths or temperature shift data to provide estimates for the earliest time that the fertile window might open.
Not all Symptothermal Methods have calculation rules. Calculation rules help to make the Symptothermal Method very safe, so I recommend all charters in times of normal fertility use a Symptothermal Method that has clear calculation rule protocols.


How Effective Is The Symptothermal Method?
There are two types of contraceptive effectiveness: perfect use, and typical use.
Perfect use effectiveness is how well the method works if you use it correctly and consistently, every single time. Perfect use effectiveness rates are calculated in clinical trials. A clinical trial is a scientific study that follows participants in real-time (or close to it). The highly controlled nature of clinical trials means that the perfect use effectiveness rates are as accurate as possible and reflect a best case scenario.
Typical use effectiveness is how well the method works for real people in the real world where mistakes and carelessness can and do occur. While typical use rates can be calculated from clinical trials, scientists prefer calculating them from large population-based surveys. Using such large surveys of people across a wide range of demographics more accurately reflects a real world scenario. Scientists prefer not to use typical use rates from clinical trials because the participants are likely influenced by lots of contact with the researchers. In addition, the participants of clinical trials are unlikely to fully reflect the large range of different demographics that will use the contraceptive method in real life.
For example: If you took the Pill consistently every single day without ever missing a day, and you always took it without fail at the exact same time every single day, the Pill would be close to 99.7% effective for you. If you took the Pill pretty consistently but forgot a day here and there, and often forgot to take it until a few hours later than you should, the Pill would be closer to 93% effective for you. This is the difference between perfect use and typical use effectiveness.


Typical use effectiveness is impacted by the level of user involvement. Contraceptive methods with a high level of user involvement usually have higher typical use failure rates. This is because there is more scope for user error. This includes contraceptive methods such as condoms, withdrawal, diaphragms, the Pill and the Symptothermal Method.
Contraceptive methods with a low level of user involvement usually have a lower typical use failure rate. This is because there is hardly any scope at all for user error. For example, hormonal IUD’s have perfect use and typical use failure rates that are identical. This is because once the IUD is inside your uterus, you don’t have to do anything to ensure that it is effective (apart from checking your IUD strings are in place each month).
In this diagram, you can see that as the level of user involvement increases, the typical use failure rate also increases.
The Symptothermal Method has a high level of user involvement compared to other methods of contraception such as the IUD or implant. More user involvement means that there is more scope for user error. The Symptothermal Method is very unforgiving of imperfect use; by definition, if a mistake is made it will result in unprotected sex during the most fertile days of the menstrual cycle.
Because of this, it’s important to take the learning process seriously. The Symptothermal Method should be learned from a qualified instructor. There have been no studies done on the effectiveness of self-teaching the Symptothermal Method.
Perfect Use Effectiveness
The Symptothermal Method has been proven up to 99.6% effective when learned with a qualified instructor. This figure is based on a 2007 clinical trial1 that followed 900 German women across 17,638 menstrual cycles over 20 years. This means that the Symptothermal Method is a highly effective form of contraception when used correctly, and learned from an instructor. For reference, the combined oral contraceptive Pill is 99.7% effective with correct use, which is a difference of only 0.1%!
Typical Use Effectiveness
It’s unclear how effective the Symptothermal Method is with typical use because there are not enough real-world users to provide a clear estimate (remember that typical use effectiveness rates are usually discovered from large national surveys). The clinical trial above showed a typical use effectiveness rate of 98.2% which is very encouraging. That said, it’s unlikely this number is reflective of real-world use because it is derived from a clinical trial. Researchers caution that we cannot compare this figure to the typical use rates of other types of contraceptives which are calculated based on large population-based surveys.

Hang On.
My Doctor Told Me The Fertility Awareness Method Was Only 76% Effective?
Most typical use effectiveness rates are calculated from the United States National Survey of Family Growth (USNSFG). This is a large, population-based survey. Unfortunately, there are not enough users of the Symptothermal Method to generate a statistically valid contraceptive effectiveness estimate from the USNSFG.
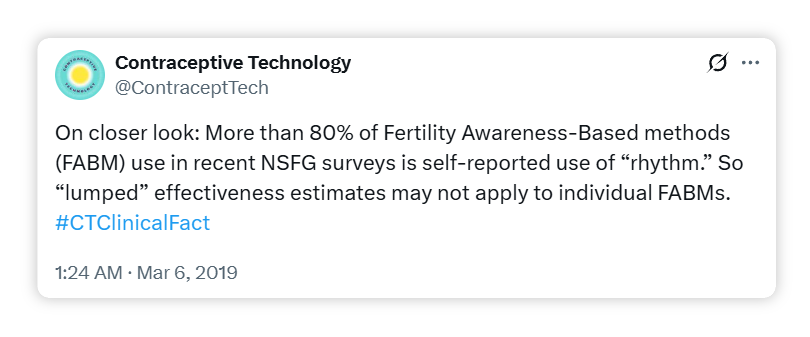
Instead, some sources choose to lump all different types of Fertility Awareness-Based Methods (FABMs) into one large group – this provides a large enough user base to generate a statistically valid result. A recent example of this is the 2006 – 2010 United States National Survey of Family Growth which provides an overarching 85% typical use effectiveness estimate for all FABMs combined (this figure is updated from an earlier USNSFG estimate of a 76% typical use effectiveness rate). The 85% typical use figure is quoted by Contraceptive Technology in their latest 21st edition published in 2018. The book Contraceptive Technology is a medical handbook used by physicians and health personnel as a resource on contraceptive counselling.
The problem with this approach of lumping all types of FABMs under one overarching typical use effectiveness rate is that it obscures the effectiveness rates of individual methods. In fact, over 80% of 2006 – 2010 USNSFG respondents were using the Calendar Rhythm method (a notoriously ineffective and outdated type of FABM). This means that any overarching typical use effectiveness rate is likely skewed significantly downward. In fact, Contraceptive Technology even tweeted about this issue:

KEY TAKEAWAYS
The Symptothermal Method is a highly effective form of natural birth control when learned from a qualified instructor, and used correctly. If possible, opt to learn a Symptothermal Method with robust calculation rules which increases the safety and effectiveness of the method.
To safely use the Symptothermal Method for natural birth control, you’ll need to consistently do three things:
- Accurately observe and chart your cervical mucus and basal body temperature.
- Accurately apply Symptothermal Method rules to identify the opening and closing of the “method-identified fertile window“.
- Modify your sexual behaviour during the method-identified fertile window.

I’ve successfully used the Symptothermal Method as my chosen form of birth control since 2016. Since then, I’ve taught hundreds of couples how to manage their combined fertility, naturally. And I’m still blown away by the whole new world that opens up when people discover how to read the language of their body.
Ready to take charge of your fertility?
Your journey starts here:
1. Frank-Herrmann P, Heil J, Gnoth C, Toledo E, Baur S, Pyper C, Jenetzky E, Strowitzki T, Freundl G. The effectiveness of a fertility awareness based method to avoid pregnancy in relation to a couple’s sexual behaviour during the fertile time: a prospective longitudinal study. Hum Reprod. 2007 May;22(5):1310-9.