The Ovarian Cycle
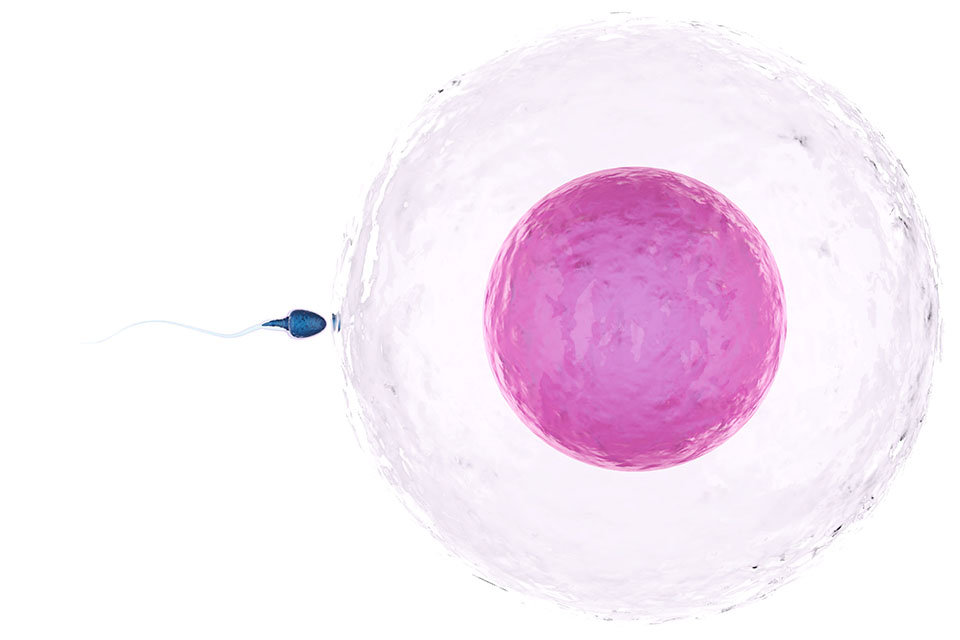
The purpose of our menstrual cycle is to pass on our genes by conceiving a child with our sexual partner. To do this, a sperm from a male has to join with one of our eggs. The human egg when mature is the largest cell in the human body and is even visible with the naked eye at around 0.1mm in diameter. Inside the egg are 23 chromosomes – half of the DNA required for the growth of a new human (the other 23 chromosomes coming from the sperm).
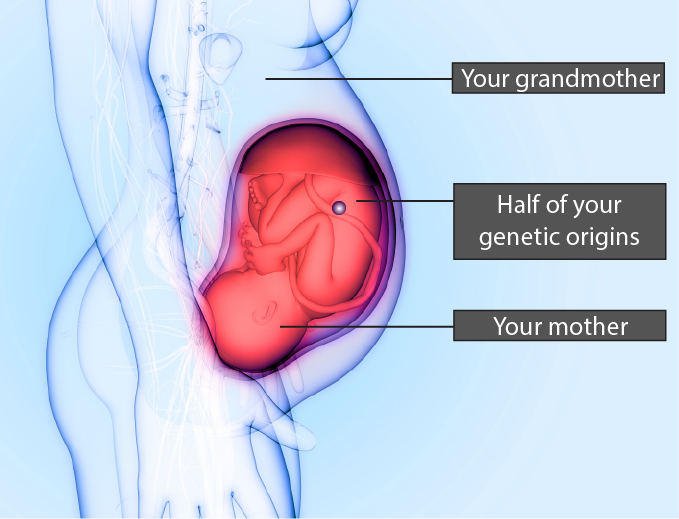
The lifecycle of the human egg actually begins in the womb. By the time you are born you have around two million immature eggs (one million in each ovary). Each egg is housed within a tiny fluid-filled sac called a follicle. Because the follicles (and therefore the eggs inside them) go through a constant process of growth and death, this number will reduce to around 400,000 by the time you hit puberty.
Our existing understanding of female fertility is that women are born with all the eggs they will ever have. Some research suggests that women may be able to grow new eggs; however, this research is still in its infancy and is mainly focused on mice. At this point in our understanding, it’s very likely that by around 20 weeks’ gestation you already have all the eggs you will ever have. This means that the origins of half of your genetic material probably first existed when your mother was a foetus inside your grandmother’s uterus!
At any one point in time we have follicles at all different stages of growth within our ovaries. This is because the growth and death cycle of follicles is a constantly occurring process throughout our lifetime and throughout our menstrual cycle. This constant growth and death cycle is known as atresia. Each menstrual cycle, a group of around 10 follicles are chosen to continue their journey of growth. Out of these ten follicles, only one will become dominant to release an egg. It takes approximately three months for a follicle to grow to the point of ovulation – the ovarian cycle discussed below is just the part of growth that occurs during the menstrual cycle.
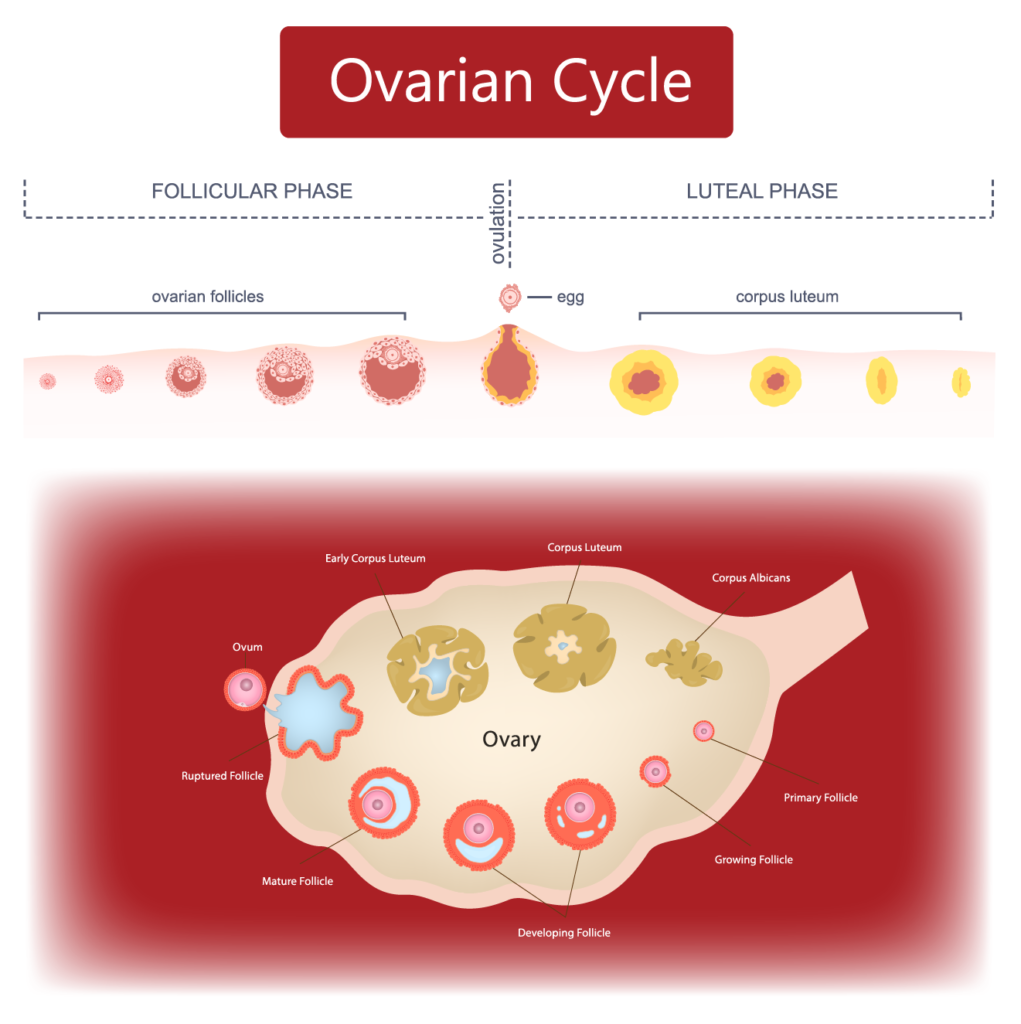
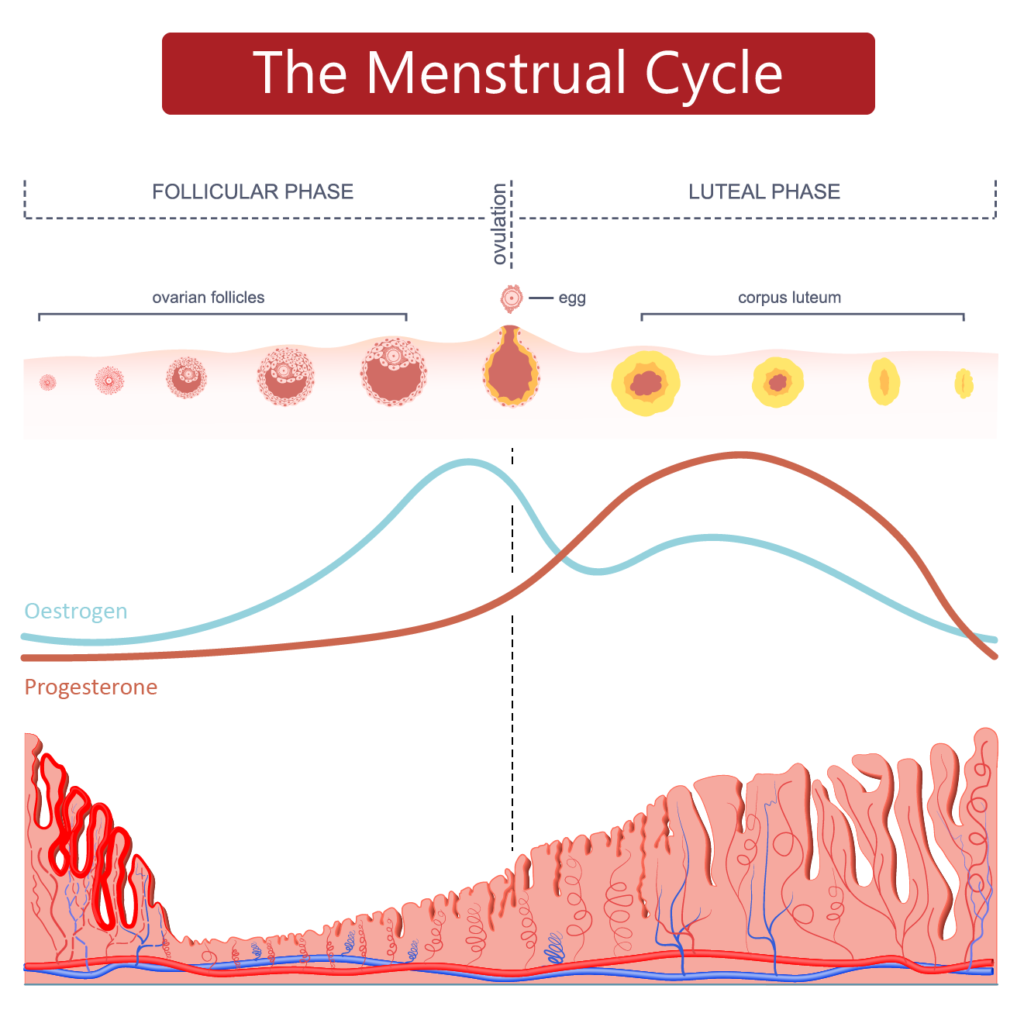
FOLLICULAR PHASE: After our period ends, a group of around 10 follicles begin to grow in your ovary. They are stimulated to start growing by a hormone called follicle stimulating hormone (FSH). Growing follicles produce the hormone oestrogen. As these follicles grow larger and larger, they produce more and more oestrogen which circulates in your bloodstream. Eventually, one follicle (the largest one) becomes dominant while the other follicles die off. This dominant follicle can grow in size up to 2cm in diameter! The dominant follicle releases peak levels of oestrogen into the bloodstream. This is why oestrogen is the dominant hormone of the follicular phase. Remember that oestrogen causes the lining of the uterus to grow.
OVULATION: Peak levels of oestrogen in the bloodstream eventually trigger a surge of luteinising hormone (LH). Luteinising hormone triggers the egg inside the dominant follicle to mature and then burst out of the follicle. This is the moment of ovulation! While we think of ovulation as a quick and explosive event, it actually takes around 15 minutes for the egg to emerge.
Once released, the egg is collected by the fimbriae of the nearest mobile fallopian tube. The cilia (hair-like projections) work to waft the egg deeper into the fallopian tube. If there are any sperm ready and waiting to fertilise the egg, this will happen in the outer third of the fallopian tube. The egg only has a very short lifespan (usually around 16 or 17 hours) but we round this up to 24 hours for the purposes of using the Symptothermal Method.
If any further eggs are released (as in the case of non-identical twins or triplets) they can only be released during the 24 hour lifespan of the first egg. This means that the maximum timespan that there could conceivably be a fertilisable egg waiting in the fallopian tubes is 48 hours each menstrual cycle.
LUTEAL PHASE: After ovulation, the follicle that the egg emerged from undergoes a transformation. The remaining cells of the follicle develop into a temporary structure known as a corpus luteum. Corpus luteum is Latin for ‘yellow body’ due to the yellowish colouring. The corpus luteum produces the hormone progesterone in large quantities. Progesterone causes the lining of the uterus to thicken and become very nutrient-rich in preparation for a potential pregnancy. Progesterone is the dominant hormone of the luteal phase.
The corpus luteum has a fixed lifespan of 10 – 16 days. If a pregnancy does not occur, the corpus luteum will begin to break down and stop producing progesterone. During the process of breaking down the corpus luteum progressively shrinks smaller and becomes known as a corpus albicans. Because progesterone (and some oestrogen) is necessary to sustain the thick endometrium, when these hormone levels drop the lining starts to slough away. This is menstruation, which happens 10 – 16 days after ovulation. During menstruation, levels of oestrogen and progesterone are at their lowest levels of the entire menstrual cycle.
If an egg is fertilised and implants into the uterine lining, the corpus luteum is ‘saved’ from breaking down. The early placental cells produce a hormone called human chorionic gonadotropin (hCG) which signals the corpus luteum to stay alive and continue producing progesterone until the placenta can take over in the second trimester. We will learn more about fertilisation, implantation and pregnancy later in the course.