Fertilisation, Implantation and Pregnancy

ACHIEVING PREGNANCY
For pregnancy to occur, a sperm must join with an egg. This is known as the process of fertilisation. Each sperm and each egg contain 23 chromosomes. Chromosomes contain DNA. DNA is passed down from each parent to their child, and contains all of the specific instructions that will make that child a unique person. For example your sex, the colour of your eyes, the shape of your nose and the length of your fingers are all encoded in your DNA. This is how parents pass on their genes to their offspring.
A very specific chain of events must fall into place for pregnancy to occur. In fact, the chance of pregnancy in any given menstrual cycle is estimated at around 25%. This number falls to around 5% once we are in our 40s.
THE JOURNEY TO THE EGG
Fertilisation occurs in the outer third section of the fallopian tubes. The journey toward this final destination is fraught with challenges for sperm. Of the 250 million sperm that are deposited in the vagina at ejaculation, only around 30 will reach the egg, and only 1 will fertilise the egg.
Sperm have to survive the acidic environment of the vagina, navigate the complex structure of the cervical crypts, find their way through the uterus to navigate the tiny opening to the correct fallopian tube, and then journey outward toward the egg. Luckily, our bodies do what they can to help!
- Cervical mucus and semen protect sperm with their alkaline pH
- The cervix widens and cervical mucus creates a ‘sperm super highway’
- The crypts of the cervix nurture hibernating sperm for around 20 hours before they move onward
- The uterus encourages sperm toward the correct fallopian tube with miniscule contractions of the endometrium
- The hair-like cilia of the fallopian tubes waft the sperm toward the outer third of the fallopian tube
- Exposure to our reproductive system initiates a biochemical reaction called “capacitation”. Capacitation causes sperm to swim faster and more vigorously. Without capacitation, sperm would not be capable of fertilising the egg.
- It’s theorised that sperm may be able to “smell” the egg with their scent receptors
Around the time of ovulation, the fimbriae of the nearest fallopian tube hover over the ovary ready for the rupture and release of the egg. Healthy fallopian tubes are relatively mobile, and in the case of women with only one ovary, it is possible for the egg to travel toward, and be collected by, the opposite fallopian tube.
The egg itself only has an average lifespan of 17 hours, so it’s important that sperm are ready and waiting in the fallopian tube in advance of ovulation.
Of the 250 million sperm that are ejaculated into the vagina; only around 30 will reach the fallopian tube to greet the egg.
FERTILISATION + IMPLANTATION
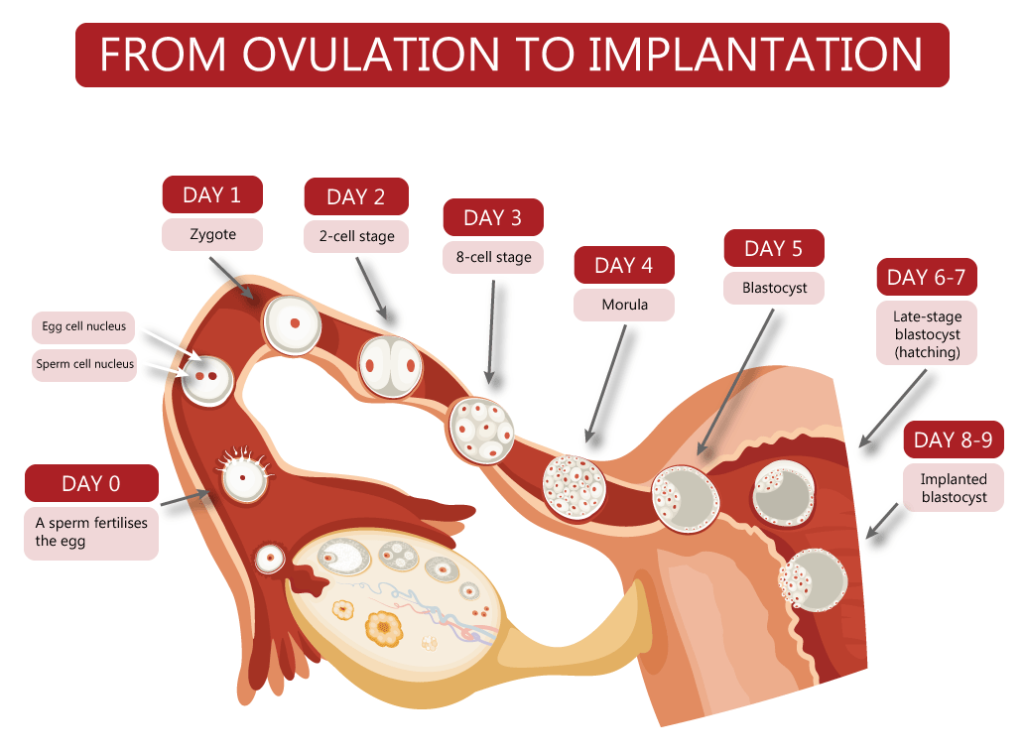
The egg arrives into the fallopian tube, and one of the waiting sperm penetrates the outer layer of the egg (known as the zona pellucida). The 23 chromosomes of the sperm and the 23 chromosomes of the egg fuse together to form a zygote. A zygote is a single cell with 46 chromosomes and all of the necessary genetic material to form a new individual.
The zygote begins to rapidly divide and move down the fallopian tube, toward the uterus. During this time it divides from 2 cells, to 4 cells, to 8 cells, and then finally around 5 days after fertilisation it reaches 16 cells. At this point it is known as a morula. It soon exits the fallopian tube, continues dividing into a blastocyst, and then implants into the uterus. Implantation usually happens around 8 – 9 days after ovulation.
PREGNANCY
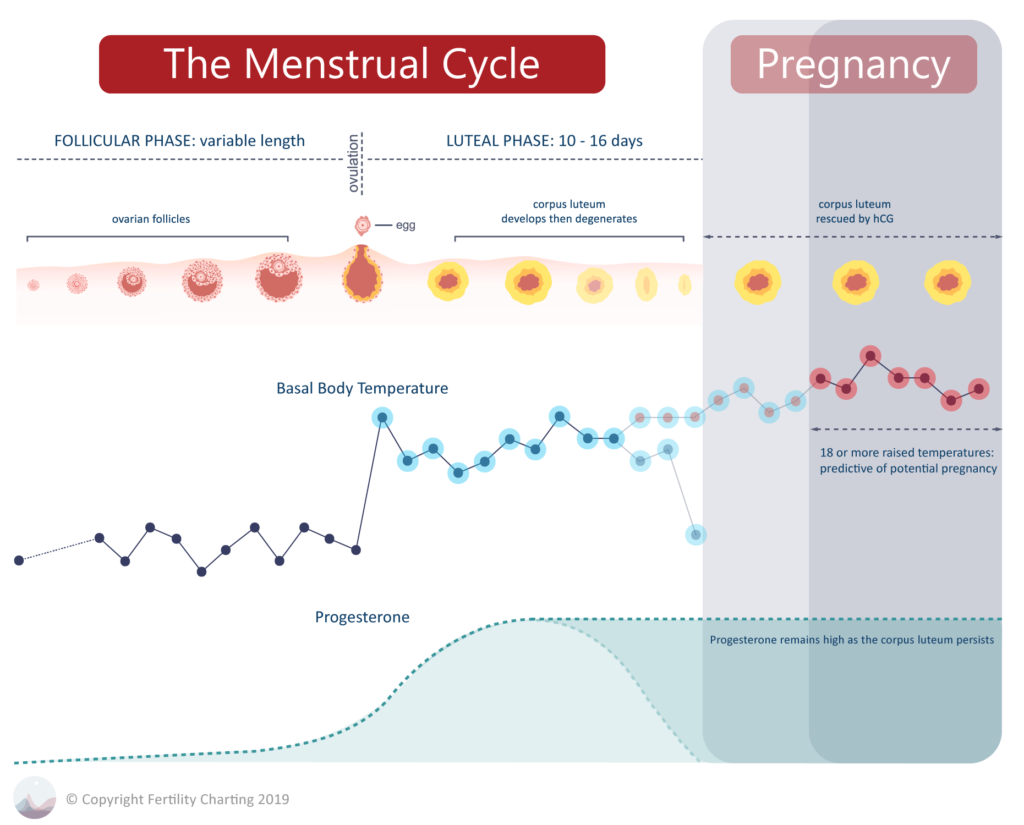
The newly implanted embryo (at this stage just a small collection of around 100 cells) begins to produce the pregnancy hormone known as hCG. hCG stands for human chorionic gonadotropin and it is produced by the early placental cells.
Remember how the corpus luteum only has a finite lifespan of between 10-16 days? Usually, if no pregnancy occurs, the endometrium will begin to break down due to falling progesterone as the corpus luteum disintegrates.
In the case of a pregnancy though, the release of hCG signals the corpus luteum to remain alive and continue producing progesterone. This ensures that the endometrium is stable and will continue to grow and thicken to nurture the new embryo.
The placenta will eventually take over from the corpus luteum to produce its own progesterone in the second trimester of the pregnancy.
PREGNANCY CHARTS
In a pregnancy chart, temperatures remain high as progesterone levels are rescued by hCG. The endometrium does not break down and menstruation does not occur. A chart with over 18 raised temperatures is a good indication that pregnancy has likely occurred.
Unfortunately, our charts do not offer any other hints that pregnancy is likely. 18 or more raised temperatures is the only predictive value that our charts provide for identifying a pregnancy. Despite this, it’s common to hear myths such as:
- A pregnancy chart will always show a triphasic temperature pattern (three levels of temperatures), or
- A pregnancy chart will always show a lot of mucus in the luteal phase
Unfortunately, none of these are true for every person. There is nothing that can confirm a pregnancy except:
- An at-home pregnancy test, or
- A blood test at your doctors office.
MISCARRIAGE
A miscarriage occurs when a pregnancy is lost before 23 completed weeks. It’s estimated that 1 in 4 pregnancies end in miscarriage, and the majority of these cases are due to chromosomal abnormalities in the embryo. This means that the majority of miscarriages occur for reasons that are completely out of our control and are nobody’s fault. In the case of miscarriages due to chromosomal abnormality, the body ends the pregnancy when it is clear that the foetus would not be viable.
Always make sure to follow up as soon as you can with a health provider if you experience bleeding or cramping in early pregnancy. If you are experiencing a miscarriage it is important that your health provider checks that the miscarriage is complete and all tissue has left the uterus. This is important because an incomplete miscarriage (where foetal tissue remains in the uterus) can cause serious infection.
Miscarriages can be extremely traumatic for women and their partners, on both a physical and mental level. Unfortunately, our society lacks supportive narrative, rituals and outlets for processing a miscarriage. Because of this, miscarriage is often endured silently. Working through your experience in a therapy modality that feels appropriate may help you (i.e. talk therapy, art therapy, ritual, journaling, counselling or other). Make sure to take all the time you need to allow yourself to move through this journey at your own pace. There is no rush or timeline that you need to adhere to. You may wish to alert your friends, family and colleagues to the fact that you will need extra support throughout this time.
The following Australian organisations provide information and support that may be useful for you if you are experiencing a miscarriage:
Pink Elephants: https://miscarriagesupport.org.au/
SANDS: https://www.sands.org.au/miscarriage
Bears of Hope: http://www.bearsofhope.org.au/
Pregnancy, Birth & Baby: https://www.pregnancybirthbaby.org.au/emotional-support-after-miscarriage
Miscarriage for Men: https://raisingchildren.net.au/pregnancy/miscarriage-stillbirth/miscarriage/miscarriage-for-men
PANDA: https://www.panda.org.au/info-support/during-pregnancy/adjusting-to-change/loss-and-grief