Navigating the Fertile Window: Barrier Methods
BARRIER METHODS: When Abstinence Isn’t An Option
While abstinence during the fertile window is preferable from an effectiveness point of view, many couples prefer not to give up PIV sex during this time.
This is a valid decision, and the Symptothermal Method can still be very safe when barriers are used during the fertile window.
Barrier methods of contraception include any methods where a physical barrier separates the sperm from the female reproductive tract. Common barrier methods can include condoms, diaphragms, cervical caps and sponges. Withdrawal (the “pullout” method) is not a barrier method but is included in this section as it also separates sperm from the female reproductive tract.
The most important thing to be aware of when using a barrier method during the fertile window, is that should the barrier method break or malfunction there is a very high risk of pregnancy. For example, if the condom breaks while you are in the fertile window, you have essentially just had unprotected sex during the most fertile week of your entire menstrual cycle!
If you have an accident with your barrier method, it’s important that you’re familiar with how to obtain emergency contraception in your area. It’s also important that both you and your partner have spoken in advance about how to handle this situation.

MALE CONDOMS
The male condom is a sheath that is placed over the erect penis. It acts as a physical barrier to prevent ejaculate from contacting the vulva and vagina.
Male condoms can protect against unintended pregnancies. Some types of male condoms (latex, polyisoprene and polyurethane) can also protect against the transmission of STIs.
How effective are condoms?
With perfect use, male condoms are 98% effective. With typical use, male condoms are 87% effective.
Considerations
- As with most barrier methods, there is a large scope for user error.
- There are different types of condoms made from different materials and each must be carefully paired with an appropriate lubricant
- Condoms are damaged by sunlight and excessive heat. Do not store them in the glovebox of your car, the pocket of your jeans, or your wallet for long periods of time.
- Condoms are not reusable and can only be used once.
- It may take some practice for your partner to learn how to correctly put on a condom.
Materials
Condoms come in four types of materials:
- Latex rubber
- Polyisoprene (synthetic latex)
- Polyurethane
- Lambskin (no protection against STIs)
Those with a latex allergy must avoid latex condoms. If you have a severe latex allergy, you may also want to avoid Polyisoprene condoms (which are made from a synethic type of latex. Polyisoprene is usually safe if you have a latex allergy, but if the allergy is severe you may want to avoid).
Lambskin condoms provide protection against pregnancy but they do not protect against the transmission of STIs.
Non-latex condoms (made from polyisoprene / polyurethane / lambskin) often have other benefits including increased heat transfer between partners and increased sensation due to their thinner material.
Lubrication
Oil-based lubricants (such as coconut oil, Vaseline, or massage oils) can damage latex and polyisoprene condoms and cause them to break. Never use oil-based lubricants with latex or polyisoprene condoms.
If in doubt, use a water-based lubricant.
Cannot be combined with:
Male condoms cannot be combined with female condoms. This is because the friction of the two condoms against each other can cause the material to quickly degrade.
Vegan?
If you’re vegan and looking for a condom brand that you can work with, here in Australia Jonny is a great choice. They are not latex-free, but are free of all animal products: https://jonny.com.au/.
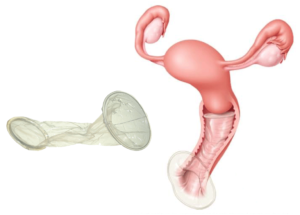
INTERNAL (FEMALE) CONDOMS
The internal (or female) condom is a nitrile sheath that has a soft ring at each end. Nitrile is a type of synthetic rubber. It is inserted into the vagina prior to having sex. The outer ring also covers part of the vulva. The female condom acts as a physical barrier to prevent ejaculate from contacting the vulva and vagina.
Internal condoms can protect against STI’s as well as unintended pregnancies when used vaginally.
How effective are internal condoms?
With perfect use, internal condoms are 95% effective. With typical use, internal condoms are 79% effective.
Considerations
- There is a high learning curve with internal condoms which means that you’re more at risk of having an accident during the first five uses of the product.
- You must be comfortable placing the product internally into the vagina
- Internal condoms are more expensive than external condoms
- Internal condoms are very visible during sex
- Internal condoms can be placed in the vagina 8 hours in advance of having sex
- Internal condoms have better heat transfer between partners compared to external condoms.
Lubrication
Internal condoms can safely be combined with water, oil and silicone based lubricants.
Cannot be combined with:
Internal condoms cannot be combined with external condoms. This is because the friction of the two condoms against each other can cause the material to quickly degrade.
Internal condoms cannot be combined with diaphragms or cervical caps. This is because the inner ring of the internal condom would likely be disrupted by the presence of a diaphragm or cervical cap.

DIAPHRAGMS AND SPERMICIDE
Diaphragms are reusable silicone domes that the user fills with spermicidal gel before placing into the vagina. When in position, diaphragms sit over the cervix to block sperm from travelling into the uterus. The spermicidal gel is held in place by the diaphragm. The gel bathes the cervix and acts as a mechanical barrier to stop sperm from entering the cervix. Diaphragms stay in place because part of their outer rim hooks into the retropubic niche (the niche behind your pubic bone). Diaphragms do not protect against STIs but can protect against unintended pregnancies.
There are two main types of diaphragms:
- Traditional fitted diaphragms
- Newer “one-size-fits-all” diaphragms
Traditional fitted diaphragms require an appointment with a healthcare provider who has training in how to use a “fitting kit”. The fitting kit is a set of different sized diaphragms that the provider tests on you to check which size is the right fit. The most well-known fitted diaphragm is the Milex Omniflex, which comes in 8 different sizes ranging from a 60mm – 95mm diameter.
More recently, a new “one-size-fits-all” diaphragm has been released called the Caya. In many countries (including Australia) the Caya is now the only diaphragm available to purchase from reproductive health clinics (as fitted diaphragms have been phased out). The Caya is said to fit around 87% of users. It is not suitable for those who would have used a Milex 60mm or smaller, or a Milex 85mm or larger.
Although the Caya is a “one size fits all” diaphragm, it still requires a visit to your nearest reproductive health clinic. A trained practitioner will need to check that the Caya will be suitable for your anatomy, and they will also need to teach you how to use it.
For those that do not want to use the Caya, it is still possible to find a way to use a traditional fitted Milex diaphragm. Some Australian reproductive health clinics still have their fitting kits which they can use to tell you which size Milex would best suit your anatomy. You can then purchase a Milex online and have it shipped to Australia from overseas.
In future: It is likely that the Milex will be phased out over the coming years. Kessel Medintim (the German company who produce the Caya diaphragm) is currently in the process of designing and manufacturing a modern fitted diaphragm which will be known as the Singa. The Singa will likely replace the Milex as it will have all benefits of a traditional fitted diaphragm in addition to a new and improved modern design.
https://www.medintim.de/singa-production-and-distribution-of-the-new-diaphragm/
How effective are diaphragms?
There is slightly less evidence available for the effectiveness of the Caya diaphragm than traditional fitted diaphragms.
A small study published in 2015 followed just under 400 women for only six months. Contraceptive effectiveness rates are usually calculated over 12 months, so the study authors had to extrapolate their findings for 12 months. They estimated that the Caya has a typical use effectiveness of 82.6% and a perfect use effectiveness of 83.7%.
Traditional fitted diaphragms have slightly more evidence to support their use. A 2007 study followed traditional diaphragm users for up to 12 months and showed a typical use effectiveness of 83.3%, and a perfect use effectiveness of 95.3%.
Official sources quote overarching effectiveness rates for both traditional fitted and modern single-size diaphragms of 83% with typical use and 84% with perfect use.
Considerations
- Will require a visit to a trained practitioner to be sized for fitting and taught how to correctly insert and remove the diaphragm
- You must be comfortable placing the diaphragm internally into the vagina
- Diaphragms are more expensive than male and female condoms; however, they can be reused for up to two years
- Purchasing spermicide (Caya/Contragel) will be an ongoing cost
- With additional application of spermicide, the diaphragm can be used for multiple sexual encounters
- The diaphragm is not visible to the male sexual partner
- The diaphragm can be placed in the vagina up to 2 hours in advance of having sex
- The diaphragm must be left in for 6 hours after sex
- The diaphragm cannot stay in the vagina for longer than 24 hours
- Diaphragms should not be used for at least 6 weeks after giving birth
- After pregnancy, miscarriage or abortion you will need to be resized as the cervix often changes shape during these events
- If using a traditional fitted diaphragm, it needs to be resized if you experience a weight change of over 5kg
- Contragel/Cayagel may make it more difficult to distinguish your normal cervical mucus pattern

Diaphragms Must Be Used With Spermicide
Diaphragms are designed to be used with spermicide (the shape of the diaphragm is specifically to hold spermicide up against the cervix).
Traditionally, most spermicides are made with an ingredient known as “Nonoxynol-9”. N-9 is highly damaging to sperm (hence it’s use in contraceptive products). Unfortunately, N-9 is also damaging to the cells that line the vagina.
If you are going to use a diaphragm, it’s recommended to use Contragel or Cayagel as opposed to traditional N-9 spermicide.
Contragel and Cayagel are the exact same product with different names. The gel is thick and viscous and has a low pH value. The acidity of the gel makes it difficult for sperm to survive. The gel is also so thick that sperm struggle to penetrate it.
During clinical trials, Contragel/Cayagel has been shown to be just as effective (if not more so) than traditional N-9 spermicides.
Contragel/Cayagel can be purchased online if it is not available for sale in your country.
Lubrication
It is recommended to use a water-based lubricant with your diaphragm. Oil-based lubricants can also be used although water-based are generally considered safer.
Diaphragms are made of silicone; therefore it is important that you do not use silicone-based lubricants. The silicone lubricant can degrade and break down the silicone diaphragm with repeated friction.
Cannot be combined with:
Diaphragms cannot be combined with cervical caps or female condoms as these methods all require use of the space around the cervix.
Traditionally, diaphragms were made of latex and it was therefore not safe to combine male condoms with diaphragms (combining multiple latex methods would weaken the latex and put both methods at higher risk of breakage). Now that diaphragms are made of silicone, it is fine to combine male condoms with diaphragms.
Many male condoms come with a small pre-loaded coating of a silicone-based lubricant; however, this small amount is not considered to pose any serious risk to the effectiveness of either device.
Best practice guidelines are to check your diaphragm after each use. You can check for leaks by filling your diaphragm with water. You can check for weaknesses by holding up your diaphragm to the light.

CERVICAL CAPS AND SPERMICIDE
Cervical caps are reusable silicone devices that are shaped like a sailors hat. They have a dome that fits directly over the cervix, and a wide brim that lodges up against the vaginal walls to assist in keeping the cap in place. There is also a thin silicon strap that can be used to remove the device. Cervical caps are designed to be used with spermicide. They come in three different sizes depending on whether you’ve ever previously been pregnant or given birth.
There is one available brand of cervical cap worldwide: the Femcap.

How effective is the Femcap?
A 1999 study followed approximately 300 women for 28 weeks to compare the effectiveness of the Femcap to traditional fitted diaphragms. The Femcap was less effective than traditional diaphragms. It was found to have a 6-month typical use effectiveness of 86.5% and a perfect use effectiveness of 88.9%. The study authors extrapolated their 6-month results to give a 12-month typical use effectiveness estimate of 77.2%.
Since this study, the creators of Femcap have changed their design slightly, so it is unclear how relevant these estimates are to the new design.
The verdict? We don’t have as much data to support the safety of cervical caps as we do for diaphragms. Additionally, the Femcap is less effective for women who have previously had a vaginal birth.
Considerations
- Will require a visit to a trained practitioner to be sized for fitting and taught how to correctly insert and remove the Femcap
- The Femcap is more difficult to insert/remove than a diaphragm
- You must be comfortable placing the Femcap internally into the vagina
- The Femcap is more expensive than male and female condoms; however, it can be reused for up to one year
- Purchasing spermicide (Caya/Contragel) will be an ongoing cost
- The Femcap is not visible to the male sexual partner
- The Femcap can be kept in place for up to 48hours during which no further spermicide needs to be added
- The Femcap must be left in for 6 hours after sex
- The Femcap causes less urinary tract infections than diaphragms
- The Femcap should not be used for at least 6 weeks after giving birth
- After pregnancy, miscarriage or abortion you will need to be resized as the cervix often changes shape during these events
- Contragel/Cayagel may make it more difficult to distinguish your normal cervical mucus pattern
Spermicide
The Femcap should be used with Cayagel or Contragel.
Lubrication
It is recommended to use a water-based lubricant with your FemCap. Oil-based lubricants can also be used although water-based are generally considered safer.
Cervical caps are made of silicone; therefore it is important that you do not use silicone-based lubricants. The silicone lubricant can degrade and break down the silicone cervical cap with repeated friction.
Cannot be combined with:
The Femcap cannot be combined with a diaphragm or female condom as these methods all require use of the space around the cervix.
Traditionally, cervical caps were made of rubber and it was therefore not safe to combine male condoms with cervical caps (combining multiple latex methods would weaken the latex and put both methods at higher risk of breakage). As the Femcap is now made of silicone, it is fine to double-up with a male condom.
Many male condoms come with a small pre-loaded coating of a silicone-based lubricant; however, this small amount is not considered to pose any serious risk to the effectiveness of either device.
Best practice guidelines are to check your Femcap after each use. You can check for holes by filling your Femcap with water. You can check for weaknesses by holding up your Femcap to the light.

CONTRACEPTIVE SPONGE
Contraceptive sponges are single-use polyurethane devices that contain around 1 gram of N-9 spermicide. They are placed into the vagina where their dimpled shape allows them to fit snugly around the cervix. They are only available in one size, and once in the vagina can protect against unintended pregnancy for up to 24 hours.
As a Symptothermal Method instructor I do not recommend contraceptive sponges as they contain the harmful N-9 spermicide which can be damaging to the cells that line the cervix and the vagina. In addition to this, contraceptive sponges do not have high effectiveness rates, and can be particularly ineffective for those who have previously given birth.
The verdict? AVOID.

WITHDRAWAL
Withdrawal (formally known as coitus interruptus) is where the male partner withdraws his penis from the vagina before he ejaculates. Withdrawal is sometimes known as the “pull-out” method. Withdrawal does not protect against STIs but can protect against unintended pregnancies.
How effective is it?
Withdrawal is estimated to be 96% effective with perfect use, and 80% effective with typical use.
Withdrawal is not well studied so there is some uncertainty about the perfect-use effectiveness rate of this method of contraception. The key issue is that pre-ejaculatory fluid (pre-cum) can sometimes contain live sperm – this means that you could be exposed to your partners sperm well before he actually withdraws his penis to ejaculate. If you choose to use withdrawal you should be aware that there is the possibility of sperm being present in pre-cum.
Considerations:
While pre-cum doesn’t originally include sperm, it is hypothesised that it may collect “leftover” sperm from previous ejaculations as it travels through the urethra. There has been minimal and conflicting research on the presence of sperm in pre-cum. A 2003 study concluded that tests on a cohort of 12 men showed no sperm present in pre-ejaculatory fluid. More recently, a 2011 study of 27 men showed that 41% of the participants had small numbers of motile sperm in their pre-ejaculatory fluid, meaning there was a very small risk of pregnancy. If you would like to use withdrawal, you should follow the below guidelines:
- When the male feels he is about to ejaculate, the penis should be withdrawn from the vagina, and the ejaculate should not land anywhere near the woman’s genitals.
- For the highest possible effectiveness, it’s recommended that the male withdraws his penis from the vagina at least a few minutes prior to ejaculation. Leaving it until the very last second can be risky and increase the chances of accidental transmission of ejaculate into the vagina or onto the vulva.
- Withdrawal is not recommended for men who cannot reliably withdraw prior to ejaculation (i.e. those who are sexually inexperienced or are not confident in their ability to feel when ejaculation is imminent.
- Pre-ejaculate can be released just after the erection is achieved, and just before ejaculation occurs. The man may not feel the pre-ejaculate being released.
- The man should urinate between each sexual encounter and be sure to wipe off the tip of the penis. Urine is acidic and may help to kill off any sperm that remain in the urethra from the previous ejaculation.
Can be combined with:
Withdrawal can be combined with all other barrier methods of contraception. Withdrawal is an easy way to increase the effectiveness of your chosen barrier method by “doubling up”. It’s highly recommended that if you will not be abstaining during the fertile window, that you add withdrawal to whichever barrier method you will be using. For example, if you decide to use male condoms during the fertile window, it’s a good idea to also have your partner practise withdrawal for extra safety during this time.

Fun fact:
One of the largest studies on the presence of sperm in pre-cum found that the study participants either consistently had sperm in their precum, or consistently did not. It’s hypothesised that some men may be predisposed to having sperm in their pre-cum, while others may not.
If you would like to try and test your partners pre-ejaculate fluid for the presence of sperm, you can purchase a microscope online. Sperm can be viewed at 400x magnification so make sure to purchase a microscope that has at least this level of magnification. Any magnification over 1000x is unnecessary and won’t add any accuracy to what you see.
A great option is the Micra First Step Self Fertility Checkup Kit for Men. These can often be found on eBay or Amazon and are designed specifically for checking sperm. It’s recommended to first check your partners ejaculate so that you have a baseline and are familiar with what the sperm look like under magnification. Then, you can check your partners pre-cum a few days later (you can try a few different versions where your partner does/does not urinate before you check his precum).
If your partner is comfortable seeing his sperm with his own eyes, then this can be a fun and interesting experiment to try. I’ve yet to meet a single person who managed to see any sperm in their partner’s precum using a microscope – let me know if you have any luck!